Genetics And Predisposing Factors
Autoimmune hepatitis is thought to result from an environmental trigger in a genetically predisposed individual, leading to loss of tolerance of T lymphocytes with subsequent hepatocyte attack.
It is a polygenic disease and does not follow a Mendelian distribution. Therefore there is no need to screen family members of patients with AIH. There is a strong genetic association with the alleles of the major histocompatibility complex class II. The presence of human leukocyte antigen genes HLA DRB1*03 and HLA DRB1*04 predisposes to AIH type 1 and affect the disease course and response to treatment. Individuals who are positive for HLA DRB1*03 are younger, respond less favorably to corticosteroid therapy, and progress more often to liver failure. On the other hand, the presence of HLA DRB1*04 is associated with higher rates of concomitant autoimmune disorders.
Autoimmune hepatitis can also be associated with autoimmune polyendocrinopathy candidiasis ectodermal dystrophy syndrome, an autosomal recessive disease characterized by hypoparathyroidism, adrenal insufficiency, and chronic mucocutaneous candidiasis. Autoimmune polyendocrinopathy candidiasis ectodermal dystrophy is the only AIH-associated disease that follows a Mendelian pattern of inheritance and genetic counseling should be offered for patients and family members.
Table 1: Drugs Associated With Drug-Induced Autoimmune-Like Hepatitis
| Association |
|---|
You May Like: Can Drinking Cause Hepatitis C
Why Do We Treat Autoimmune Hepatitis With Steroids And Azathioprine
Despite the limitations of these early trials, prednisone ± azathioprine remains the mainstay of treatment for AIH, several reports showing high remission rates and favourable outcomes in both adult and juvenile AIH.
Of note, azathioprine monotherapy, though unsuccessful in the induction of remission, is effective in adults as maintenance therapy, at a dose of 2 mg/kg per day. A 5-patient report suggests that it may be effective also in children. In a recent retrospective series, 87% of 66 children with AIH were reported to maintain sustained biochemical remission in association with low 6-thioguanine nucleotides levels on an azathioprine dose of 1.2-1.6 mg/kg per day with or without associated steroids.
Do Medicines Used To Treat Autoimmune Hepatitis Have Side Effects
Medicines for autoimmune hepatitis can cause side effects. Your doctor will monitor any side effects and help you manage them while you take these medicines. Your doctor also may adjust the doses or change the medicines you take. You may need to stop taking corticosteroids or azathioprine if you have severe side effects.
Side effects of corticosteroids may include
- changes in how you look, which may include weight gain, a fuller face, acne, or more facial hair
Corticosteroids and azathioprine suppress, or decrease the activity of, your immune system, which increases your risk for infections. These medicines can also increase your risk of developing cancers, especially skin cancers.
Don’t Miss: How Can You Catch Hepatitis B
Do Patients Recover From Autoimmune Hepatitis Treatment
Autoimmune hepatitis is a chronic condition, and while it can be managed, it usually cannot be cured. It is possible to achieve remission from autoimmune hepatitis with the use of steroids. However, most individuals will require treatment for the rest of their lives. The 10-year survival rate for people being treated for autoimmune hepatitis is between 83.8%94%. Without treatment, the survival rate falls to 50%60%.
Signs & Symptoms Of Autoimmune Hepatitis

Most cases of early autoimmune hepatitis have no symptoms and can only be detected by routine blood tests . The symptoms of autoimmune hepatitis differ depending on its severity and may include:
- Itchy skin, dark urine, pale stools, disorientation, abdominal swelling, and leg swelling if the disease gets worse
Read Also: Hepatitis B Symptoms And Treatment
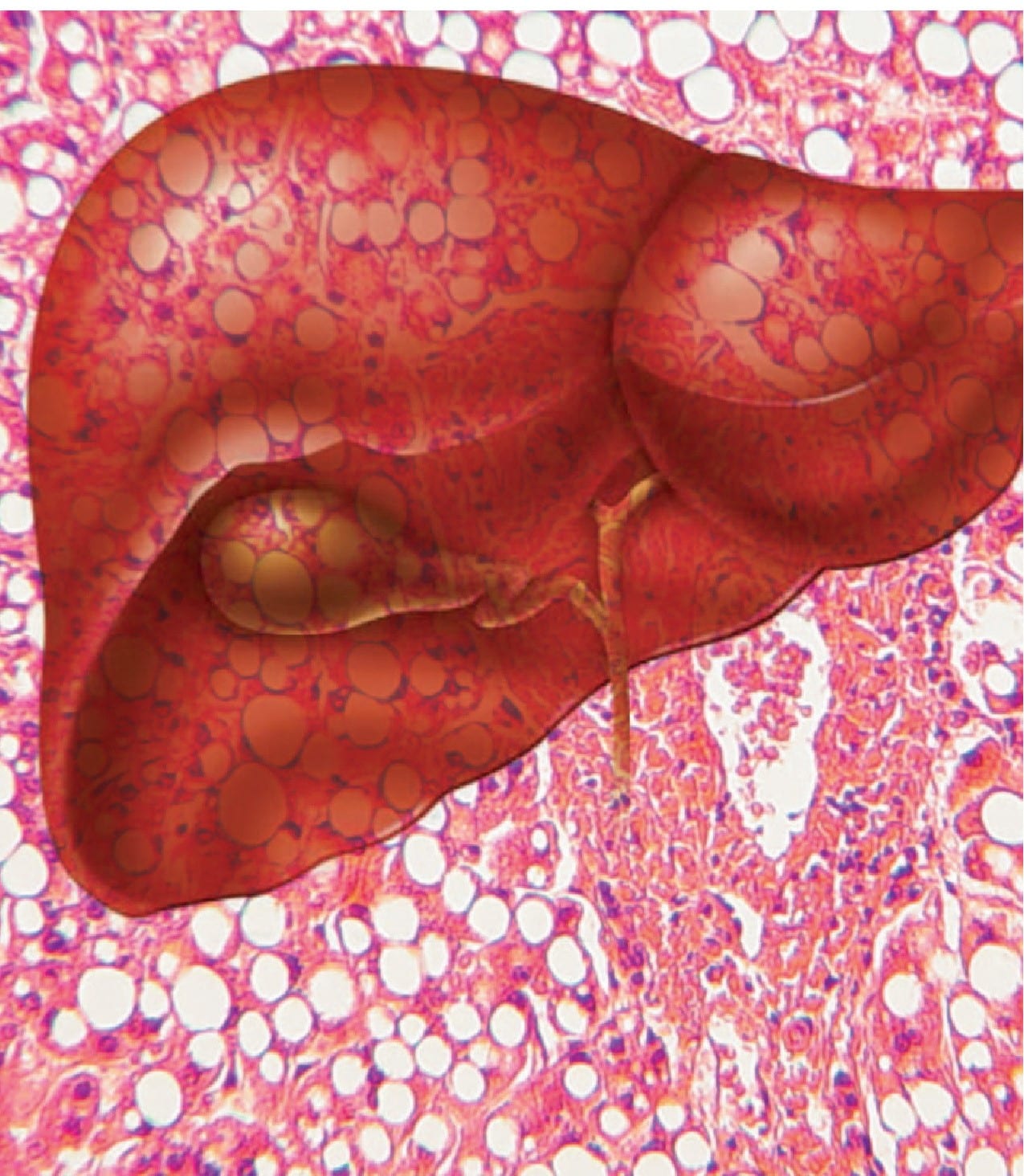
When The Liver Is Under Attack
In people with autoimmune hepatitis, immune cells inappropriately mistake the liver’s normal cells as abnormal and attack them. Over time, this can lead to inflammation, scarring , impaired liver function, and even cirrhosis , which can result in liver failure, and death if not treated. Some people may eventually need a liver transplant. The liver disease specialists at NewYork-Presbyterians Center for Liver Disease and Transplantation are experienced in diagnosing and treating autoimmune hepatitis.
Boost Up Your Glutathione
Glutathione is considered the master anti-oxidant within the body and is produced by every cell in the body where it functions to protect our DNA. Glutathione is our cells security guard that protects the cellular components from outside free radical attack. Longevity scientists now believe that the level of glutathione in our cells has a direct relationship with how long we will live .
Glutathione plays a very important role in establishing immune tolerance . Studies have demonstrated that glutathione enhances the function of T cells and modulates immune activity . In this way, optimizing glutathione levels are extremely important for reducing collateral damage associated with inflammation and autoimmune reactions .
This article goes into more detail on glutathione and its role in reducing inflammation. Hopefully, this article has given you hope and several major action steps to reduce inflammation and heal autoimmune disease.
Read Also: What Is Hepatitis B Vaccine For
Recommended Reading: How To Reduce Hepatitis B Viral Load Naturally
Is It Contagious Or Hereditary
It is absolutely not contagious. It is generally not considered an inherited disease but a tendency to autoimmune diseases may run in some families. That is, children of patients with autoimmune hepatitis may be at slightly increased risk of developing autoimmune diseases of the thyroid or liver or arthritis. The risk, however, is only slightly greater than the normal population and thus genetic counselling is not necessary.
What Are The Current Treatment Options
Very mild cases or inactive phases of the disease may not require treatment. However, for more serious cases, treatment to fight acute episodes is important.
For many individuals, lifelong medication use may be required to keep the bodys autoimmune response under control and preserve liver health.
The two main medications used to treat autoimmune hepatitis are:
- prednisone: a corticosteroid
- azathioprine: an immunomodulator or steroid-sparing agent
Other medications may be added in severe cases. If medications are no longer effective and liver failure is likely, a liver transplant may be necessary.
If possible, your treatment should be supervised by a hepatologist, which is a physician who specializes in liver health.
Recommended Reading: The Vaccine For Hepatitis B
Treatments For Autoimmune Hepatitis
Treatment works best when AIH is diagnosed early. The goal in treating AIH is to slow or stop the bodys immune system from attacking the liver. The medications used are immunosuppressants, such as prednisone and Imuran® . Physicians usually prescribe a high initial dose of prednisone, and then taper it down progressively as symptoms and liver enzymes improve. Most people will need to take medication for the rest of their lives. Since prednisone can cause a wide range of side effects, Imuran® is often used in conjunction to allow for a lower dose of the prednisone.
Some people may go into remission, during which physicians can effectively discontinue treatment others will relapse after stopping treatment, and will then need to restart the medication and continue on long-term maintenance therapy. A few patients may eventually be tapered off the prednisone completely and stay solely on Imuran®. For those who do not respond to, or relapse from, the combination regimen, then stronger immunosuppressive agents such as mycophenolate mofetil, cyclosporine, or tacrolimus may be considered. When medications do not halt the progress of the disease, or complications from cirrhosis have developed, the remaining option is a liver transplant. Fortunately, the success rate of transplantation in people with AIH is excellent.
What You Can Do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there’s anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you’re experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you’re taking.
- Take a family member or friend along to help you remember everything that was discussed.
- Write down questions to ask your doctor.
For autoimmune hepatitis, some basic questions to ask your doctor include:
You May Like: What Type Of Hepatitis Is Curable
How To Use Prednisone And Azathioprine
There is no treatment schedule applicable to all AIH patients. The suggested algorithms and treatment schedules must be tailored to the single patient, taking into account the severity of the disease, age and co-morbidities.
The AASLD guidelines published in 2010 recommend two alternative schedules: either prednisone alone at a dose of 60 mg/d or a combination of prednisone 30 mg/d and azathioprine 50 mg/d as initial treatment, favouring the latter because of fewer steroid side-effects. However, as azathioprine can be hepatotoxic, particularly in cirrhotic and jaundiced patients, the more recent guidelines by the European Association for the Study of the Liver recommend that it is added after two weeks of steroid monotherapy , when partial disease control has been achieved. In addition, this approach avoids the problem of distinguishing between azathioprine-induced hepatotoxicity and non-response, this distinction being an important issue in clinical practice. A retrospective series of 133 adult patients reports better results with a combination of steroids and another immunosuppressant from disease presentation compared to steroids alone or steroids followed by the addition of azathioprine/other immunosuppressants. Of note, only 2% of the patients included in this study were jaundiced at presentation, possibly explaining the high remission rate on azathioprine, without hepatotoxicity.
What Causes Autoimmune Hepatitis
Experts dont know what causes autoimmune hepatitis, but it is more likely to show up in people with other autoimmune conditions, including:
- Fluid buildup in the belly
- Rectal bleeding or vomiting blood
The symptoms of autoimmune hepatitis may look like other health problems. Always see your healthcare provider for a diagnosis.
Don’t Miss: Is Hepatitis C An Std
What Are The Symptoms Of Autoimmune Hepatitis In A Child
Both Type I and Type II autoimmune hepatitis have similar symptoms. Autoimmune hepatitis symptoms can come on suddenly or may develop over time. Some children with autoimmune hepatitis do not show any obvious symptoms such children may only be diagnosed because of abnormal blood test results. When symptoms do appear, they may include:
- Pale or gray stool
- Aches in joints
What Are The Types Of Autoimmune Hepatitis
Autoimmune hepatitis is classified into several types. Type 1 autoimmune hepatitis is the most common form in North America. Type 1 can occur at any age however, it most often starts in adolescence or young adulthood. About 70 percent of people with type 1 autoimmune hepatitis are female.1
People with type 1 autoimmune hepatitis commonly have other autoimmune disorders, such as
Type 2 autoimmune hepatitis is less common and occurs more often in children than adults.1 People with type 2 can also have any of the above autoimmune disorders.
Don’t Miss: At Home Hepatitis C Test
About Autoimmune Liver Disease
Autoimmune liver diseases are typically long-lasting and recurring conditions. This means that you may experience persistent immune system attacks that destroy liver cells. As cells die, scar tissue known as fibrosis forms. Autoimmune diseases tend to progress slowly, and you may have long periods without symptoms. When scarring becomes extreme, liver function weakens and eventually may result in a condition known as cirrhosis. Cirrhosis is also known as liver failure or end-stage liver disease. The only cure for this condition is organ transplantation. While the only cure for severe cirrhosis is transplantation, we can help you manage the symptoms of the disease with medication before or instead of transplantation.
Our liver specialists work closely with other experts at Mount Sinai to provide a comprehensive approach to treating you if you have multiple autoimmune conditions. Our goal is to keep your immune system active and related symptoms under control.
Mount Sinai liver specialists work with colleagues in rheumatology, endocrinology, gastroenterology, radiology, and pathology to manage autoimmune liver disease. We use state-of-the-art methods of diagnosis and treatment.
If end-stage liver disease develops and you need liver transplantation, we have the expertise to help you. We have extensive experience treating patients with autoimmune liver disease. After living with chronic liver disease, through treatment, we can help restore your quality of life.
How Is Autoimmune Hepatitis Treated In A Child
Autoimmune hepatitis is a serious, long-lasting disease. Right now, there is no cure for autoimmune hepatitis. Fortunately, most children with autoimmune hepatitis respond well to treatment.
The goal of autoimmune hepatitis treatment is remission. This means symptoms become less severe and liver damage slows or stops. Some children are able to stop taking medicine after two or three years. These children will still need to be watched for a return of autoimmune hepatitis symptoms and other health issues.
Two main types of medicine are used to help control autoimmune hepatitis in children:
- Corticosteroids . Prednisone helps stop the immune system from attacking the liver. It also reduces liver inflammation. Budesonide is another corticosteroid that is sometimes used it has less side effects, but it is mostly given later on when the disease is under control already.
- Immunosuppressants. Azathioprine or mercaptopurine are often added to the treatment they work together with prednisone to get the immune system under control. There are other medications to suppress the immune system that can be used if the standard treatment is not working well.
Also Check: Is Hepatitis C Contagious After Being Cured
How Is Autoimmune Hepatitis Diagnosed
Your healthcare provider will look at your health history and give you a physical exam.
Some lab blood tests used to diagnose autoimmune hepatitis include:
- Liver function tests. These check for inflammation or damage to your liver.
- Complete blood count or CBC. Looks at the number and types of cells in your blood.
- Coagulation panel. This test looks at how well the clotting proteins are working.
- Electrolyte panel. Checks to see if you have an electrolyte imbalance.
- Autoimmune antibodies. These are used to see if you have autoimmune hepatitis or another liver disease with similar symptoms.
- Other liver tests. These are done to check for other possible types of liver disease.
You may also have imaging tests such as:
What Is Autoimmune Disease
One job of the immune system is to protect the body from viruses, bacteria, and other living organisms. The immune system usually does not react against the bodys own cells. However, sometimes it attacks the cells it is supposed to protect this response is called autoimmunity. Researchers think certain bacteria, viruses, toxins, and drugs trigger an autoimmune response in people who are genetically susceptible to developing an autoimmune disorder.
Don’t Miss: Hepatitis B Vaccine 3 Dose Schedule
Types Of Autoimmune Hepatitis
There are two types of autoimmune hepatitis. Type 1 autoimmune hepatitis is the most common kind in the United States, while type 2 is more commonly seen in Europe and tends to be a more severe disease. The two forms of autoimmune hepatitis are characterized by the presence of different types of antibodies, proteins released by the immune system to fight bacteria and viruses. They are:
- Type 1 is the most common, accounting for 96% of autoimmune hepatitis cases in North America. It usually affects young women who have other autoimmune conditions, such as type 1 diabetes, thyroiditis, and celiac disease. People with this type of autoimmune hepatitis have antinuclear antibodies and antismooth muscle antibody .
- Type 2 is less common in North America, making up only 4% of all autoimmune hepatitis cases. It typically affects females ages 214. Individuals with this type of autoimmune hepatitis have anti-liver kidney microsomal antibody type 1 and/or anti-liver cytosol type 1 autoantibodies.
What Is It Like To Live With Autoimmune Hepatitis
Autoimmune hepatitis is a chronic condition that may require treatment for the rest of your life. Once your liver function blood tests have returned to a healthy range, your medical team may be able to reduce your steroid use. Most individuals who are treated for autoimmune hepatitis have a good prognosis and do not experience additional complications. While you may need to take a medication every day, you can still go on to live a full, healthy life.
Don’t Miss: How Do I Know If I Have Hepatitis
What Are The Symptoms And Complications Of Autoimmune Hepatitis
Often, the symptoms of autoimmune hepatitis are minor. When symptoms do occur, the most common are fatigue, abdominal discomfort, aching joints, itching, jaundice , enlarged liver, nausea and spider angiomas on the skin. Other symptoms may include dark urine, loss of appetite, pale stools and absence of menstruation. More severe complications can include ascites and mental confusion. In 10%-20% of cases, autoimmune hepatitis may present with symptoms like an acute hepatitis.
Identifying Endpoints Of Therapy
Adverse endpoints like malignancy, death or transplantation are impractical for evaluating new therapies in PSC given the long duration of disease. Moreover, the heterogeneity of PSC makes accurate patient selection and stratification for clinical trials difficult, particularly with regard to cholangiographic pattern of disease, the presence and influence of coexisting IBD, and in those having overlapping features with AIH/IgG4-associated cholangitis.
Don’t Miss: What Are The Types Of Hepatitis
Aim And Methodology Of The Systematic Review
The aim of this review is, in its first part, to critically summarize the evidence on which standard AIH treatment is based, and, in its second part, to provide a systematic review of the published data on alternative treatments. For the purpose of the systematic review of the literature on alternative AIH treatment, publications cited in PubMed were selected using the search words autoimmune hepatitis and treatment. Citations were chosen on the basis of their relevance to the aim of this article .1). Fundamental characteristics of the abstracts judged pertinent to the review were noted, and full-length original articles were selected from the abstracts. Seventy-six articles were identified, 22 of them are not discussed in this review because of anedoctal reporting, the remaining 54 are included in Table Table11 and Table Table22 . Children/adolescents have a more aggressive disease, with a more frequent acute presentation and therefore need a different management. For this reason, the present review article discusses adult and pediatric treatment separately.