Steroid Boluses And Okt3
Numerous early studies clearly demonstrated that steroid boluses and/or OKT3 administered for graft rejection in HCV-positive patients accelerate recurrent hepatitis C .
4.1.1. Steroid Maintenance
Based on early perceptions that a steroid bolus for acute rejection accelerates hepatitis C progression, steroids were believed to increase HCV injury. Considering liver injury and the long-term side effects of steroids, steroids were routinely discontinued by 3 months in most liver transplant programs until 2002 . Another option to avoid the negative effects of steroids is to use a steroid-free immunosuppressive regimen.
In addition to early reports , two recent retrospective studies revealed that slow steroid tapering might be associated with less severe recurrent disease. The most compelling data supporting the beneficial effects of low-dose steroids is from Vivarelli et al. , who reported the results of a randomized study of rapid versus slow steroid tapering in conjunction with tacrolimus. The rates of histologic recurrence at the 1-year followup and of advanced fibrosis at the 2-year followup were significantly higher in the rapid tapering group. This important finding might resolve the controversy about the impact of low-dose steroids on the natural history of recurrent hepatitis C.
Current Status Of Ldlt
In areas with low deceased-donor organ availability like Japan, the indication of LDLT for HCV cirrhosis is similar to that of DDLT , whereas in Western countries, LDLT is conducted in an attempt to alleviate the shortage of donor organs and decrease the mortality among patients awaiting transplants, accounting for only 3% to 4% of all liver transplants .
According to the Japan Liver Transplantation Society , a total of 6097 LDLTs, comprising 98% of all liver transplants, have been performed till the end of 2010 in Japan. Among those, 3796 were adult cases including 1200 cases of HCV-related disease as a leading indication for adult LDLT. The 1, 3, 5, and 10 year survival rates of all adult LDLT and those of HCV-positive adults were 81%, 75%, 72%, and 66%, and 78%, 72%, 68%, and 59%, respectively, without difference.
In the United States, nearly 3000 LDLTs have been performed by the end of 2009, with decreased number of cases annually, comprising only 4.5% of all liver transplants .
Antiviral Treatment For Established Recurrent Hepatitis C
The most widely accepted and used strategy is initiating antiviral therapy once recurrent hepatitis C in the graft is established by liver biopsies. Initial studies of monotherapy with IFN-alpha yielded poor results, with SVR rates lower than 5% . With the addition of RBV to IFN-alpha treatment, there is a noticeable improvement in treatment outcomes with an SVR rate of 17% to 30% . More recently, several centers reported that PEG-INF/RBV treatment with an improved SVR rate which has now become an established treatment for recurrent hepatitis in HCV-positive recipients .
The recent reports of PEG-INF/RBV treatment are summarized in Table 2 . Most of the data come from uncontrolled studies with different designs regarding time to start treatment, regimen used, and followup, but treatment duration is generally 48 to 52 weeks. Therefore, the results were also very different, with SVR rates ranging 0% to 56% . These results are lower than those obtained in nontransplant populations, possibly due to the immunosuppressive status, high prevalence of genotype 1, high viral load, the difficulty in maintaining adequate antiviral doses , and the difficulty in maintaining therapy for the ideal duration.
Also Check: Does Hepatitis B Have A Cure
Liver Transplant In The Setting Of Chronic Hcv Infection
Chronic hepatitis C virus -induced end-stage liver disease, with or without hepatocellular carcinoma, is still the leading indication for liver transplant , and reinfection of grafts by HCV is the main cause of allograft loss. Most patients experience recurrence of HCV infection after LT, and such recurrence can be associated with substantially accelerated cirrhosis of the graft in as many as 30% of patients. A subgroup of patients experience fibrotic cholestatic hepatitis , a severe and extremely aggressive form of HCV recurrence characterized by rapid progression to graft failure and death. Once cirrhosis develops, the annual risk of hepatic decompensation is approximately 40%, and 10% to 25% of patients will die or require retransplantation within 5 years after the first LT. Unfortunately, the outcome of patients undergoing retransplantation is poor, and most transplant centers are reluctant to offer a second LT for patients with cirrhosis of the graft due to HCV reinfection.
Testing For Liver Cancer
Having hepatitis C increases your risk for liver cancer, so your doctor may suggest an ultrasound test of the liver every 6 to 12 months. Finding cancer early makes it more treatable. Ultrasound is a machine that uses sound waves to create a picture of your liver. Ultrasound is performed at a hospital or radiology center by a specially trained technician. The image, called a sonogram, can show the livers size and the presence of cancerous tumors.
Don’t Miss: Human Hepatic Stellate Cell Line
Immunosuppression And Recurrent Hepatitis C
It is generally accepted that over-immunosuppression, such as steroid bolus and OKT3 as rejection therapy, and maintenance immunosuppression with triple-quadruple therapies at full dose are risk factors for HCV liver injury and are associated with a poorer outcome. The optimal immunosuppressive regimen for HCV-infected patients after liver transplantation remains unclear, however, despite several advances in our knowledge regarding the impact of various medications on HCV recurrence in parallel with the development of promising new drugs.
Clinical Presentation And Diagnosis Of Alcohol
ALD is defined as a clinical histopathologic spectrum ranging from steatosis, AH, and liver fibrosis ultimately leading to cirrhosis. ALD can be difficult to diagnose clinically because many patients may not disclose alcohol use and most patients remain either asymptomatic with silently progressive disease or present with nonspecific symptoms such as fatigue. As such, patients with significant alcohol use should be evaluated for possible ALD, which includes screening with serum liver tests and ultrasonography. In patients with ALD, transaminase levels are generally below 400 IU/L, with an elevated aspartate aminotransferase to alanine aminotransferase ratio.9
Even after taking a clinical history of a patients alcohol intake, differentiating between nonalcoholic fatty liver disease and ALD can remain challenging. Because many patients may not disclose alcohol use, clinicians should have a high clinical suspicion for AH, particularly in patients who present with acute jaundice, AST greater than ALT, and high international normalized ratio. Additionally, discriminant indices, such as the ALD/nonalcoholic fatty liver disease index, have been developed to help differentiate these clinical entities.
Don’t Miss: Hepatitis C Viral Rna Quantitative Real Time Pcr
Approaches To The Treatment Of Hcv Recurrence Following Liver Transplantation
Along with the impact of the previously mentioned factors on disease recurrence and overall patient and graft survival, antiviral therapy success rates appear to be one of the most important factors.
Several strategies for HCV treatment in the setting of LT have been attempted: treatment prior to LT, immediate or perioperative prophylaxis of HCV graft infection, early pre-emptive HCV therapy and treatment of established recurrent graft disease.
There is an open debate regarding which of the previously stated options are preferable following liver transplantation. Thus far, a consensus has not been reached because these four approaches have not been prospectively compared in appropriately powered randomized trials using clinical endpoints. Unfortunately, due to the heterogeneity of end-stage liver disease, the small number of patients, and the highly complex treatment of liver transplant candidates and recipients, it is unlikely that such trials will be performed in a randomized controlled fashion. In their absence, the recommendations are guided by the results of clinical trials that assess each approach separately as well as data from the real-world and the panel members experiences.
Factors Influencing Disease Severity And/or Progression Or Survival 00179
2.5.1 HCV genotypes
Ann Surg.Gastroenterology.
Gastroenterology.Hepatology.J Hepatol.
Hepatology.Liver Transpl Surg.
Transplantation.
2.5.2 HCV-RNA levels
J Hepatol.Hepatology.Hepatology.Hepatology.Hepatology.Gastroenterology.
Hepatology.Hepatology.Hepatology.
Hepatology.Hepatology.Hepatology.
Liver Transpl Surg.
2.5.3 Necroinflammatory activity and fibrosis grading observed on the initial liver biopsy
J Hepatol.
Hepatology.Liver Transpl.Transplantation.
2.5.4 Degree of immunosuppression
Ann Surg.Hepatology.Gastroenterology.Liver Transpl.Hepatology.
Liver Transpl Surg.
Transplantation.
Ann Surg.Hepatology.Liver Transpl.
Hepatology.
J Hepatol.
Am J Gastroenterol.J Hepatol.
J Hepatol.
J Hepatol.
J Hepatol.
J Hepatol.Hepatology.Lancet.
Transplantation.
Tissue Antigens.
Ann Surg.
Hepatology.Transplantation.Gastroenterology.
Ann Intern Med.Gastroenterology.J Hepatol.Liver Transpl.
J Virol.Hepatology.
Hepatology.Hepatology.Hepatology.
J Hepatol.
Recommended Reading: Royal Canin Hepatic Dry For Dogs
The Paradox Of Rejection
The most dangerous risk for transplantation patients is rejection. This occurs when the bodys immune system attacks and destroys the transplanted organ.
Why does the immune system, which is there to protect us, try to reject the life-saving transplant? Rejection occurs because the immune systems job is to target and destroy foreign cells that pose a risk. Immune cells identify foreign cells by looking at unique molecular fingerprints on their surfaces and comparing them to the bodys own unique molecular fingerprints. In this way, the immune system distinguishes between self and non-self. A donor organ comes from someone whose cells have a different molecular fingerprint. Unfortunately, the immune system reacts as if the body has been invaded. It unleashes its destructive power to get rid of the foreign cells that it has mistakenly perceived as a threat. If not suppressed, the immune system can destroy a transplanted liver within days.
You May Also Like
Several drugs have been developed that stop or slow the rejection process. Anti-rejection drugs may be given by injection during the first several weeks and later in pill form.
You May Also Like
Natural History Of Hcv Infection
It has been estimated that 75% to 85% of individuals infected with HCV progress to chronic infection, persisting for at least 6 months after onset, with the rate of chronic infection varying by age, sex, race, and immune system status8. Long-term infection has been associated with serious clinical sequelae, including development of hepatic fibrosis, cirrhosis of the liver, portal hypertension and HCC9–11. Although the natural history of HCV infection is believed to be variable, it is estimated that up to 20% of chronically infected individuals will develop liver cirrhosis over a 20- to 25-year period, and that these individuals are at increased risk of developing end-stage liver disease or HCC9-10. Of note, progression to cirrhosis can occur rapidly, even in patients with early-stage disease12. The pathway of acute hepatitis leading to chronic persistent hepatitis, which in turn may lead to cirrhosis, can show variations, such as spontaneous resolution, or the more threatening fulminant hepatic failure or cholestatic hepatitis12.
Read Also: Can Hepatitis Cause Heart Problems
Transplantation Of Other Organs
In the THINKER trial, 10 HCV-uninfected kidney transplant recipients received allografts from genotype 1 HCV-viremic donors and were treated with 12 weeks of elbasvir/grazoprevir 100% achieved SVR . In a 1-year follow-up study that included 10 additional participants who received 12 to 16 weeks of elbasvir/grazoprevir , all achieved SVR12. Kidney function in those who received kidneys from HCV-infected donors was comparable to matched controls who received allografts from HCV-uninfected donors . A separate open-label trial similarly demonstrated 100% SVR12 with 12 weeks of elbasvir/grazoprevir therapy initiated immediately prior to transplantation in 10 HCV-uninfected kidney transplant recipients of allografts from HCV-viremic donors . Notably, organ recipients in this study received the first dose of elbasvir/grazoprevir on call to the operating room. Of the 10 patients treated, only 3 had detectable HCV viremia compared to 100% in the THINKER trial, which utilized the same regimen but initiated therapy on day 3 after transplantation.
A separate study conducted among 50 heart transplant recipients , an 8-week course of glecaprevir/pibrentasvir was initiated once viremia developed . Investigators noted a higher proportion of acute cellular rejection in the HCV-viremic vs HCV-aviremic donor study groups in the first 2 months and at 180 days . These findings raise concern about a potential association between HCV-viremic donors and rejection.
Criteria For Transplantation Referral
- MELD-sodium score: optimal timing for first referral is MELD 10, and definitely by MELD 15
- First development of any decompensation event: ascites, variceal bleeding, or hepatic encephalopathy
- HCC without metastasis or macrovascular invasion patients with HCC and cirrhosis should be referred for transplant evaluation
Read Also: Google What Is Hepatitis B
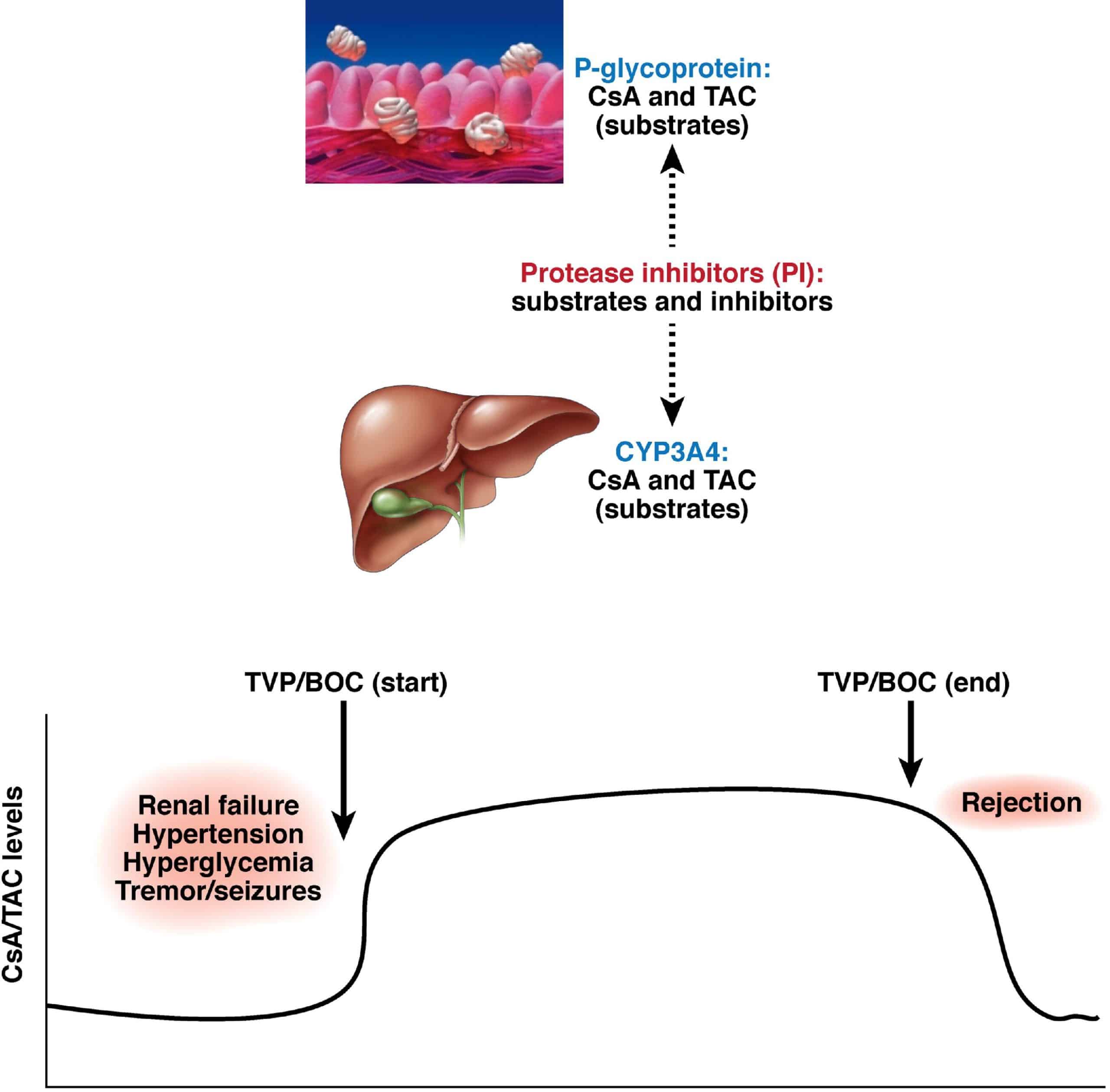
Future Therapeutic Strategies: New Daas And Ifn
For decades, HCV has successfully escaped from all efforts to generate more efficient drugs, although research efforts have been intense. Viral replication in vitro or in small-animal models could not be achieved, and functional studies were limited to chimpanzees, what caused an important drawback to DAA development. The ultimate breakthrough for HCV drug development may be dated to establishment of the HCV replicon system, what was not earlier that 1999. HCV subgenomes, which compose the nonstructural proteins NS3-NS5 linked to a selectable marker, can efficiently replicate in vitro. A few years later, a full-length isolate of HCV became available which can produce infectious viral particles in vitro. The resulting improvement in the understanding of the viral life cycle opened the doors for the development of the first-generation DAAs. Drug development was further supported by structural biology, which has provided high-resolution images of the structures of the virus, revealing additional crucial drug targets, such as NS3, NS5A, and NS5B. These images have allowed modelling of interactions between specific replication inhibitors and their targets.
With the advent of the NS5B polymerase inhibitor sofosbuvir , the NS3 PI simeprevir , and the NS5A replication inhibitor daclatasvir , three second-wave DAAs are now available and promise to be appropriate for LT patients, without severe adverse effects or negative interactions with immunosuppressants.
How Could I Get Hepatitis C
You could get hepatitis C through contact with an infected persons blood. This contact could occur by
- being born to a mother with hepatitis C
- getting an accidental stick with a needle that was used on an infected person
- having unprotected sex with an infected person
- having contact with blood or open sores of an infected person
- sharing drug needles or other drug materials with an infected person
- being tattooed or pierced with unsterilized tools that were used on an infected person
- using an infected persons razor, toothbrush, or nail clippers
You could get hepatitis C from sharing drug needles or other drug materials with an infected person.
You cannot get hepatitis C from
- shaking hands or holding hands with an infected person
- being coughed or sneezed on by an infected person
- hugging an infected person
- light-colored stools
- yellowish eyes and skin, called jaundice
When symptoms of hepatitis C occur, they can begin 1 to 3 months after coming into contact with the virus. See a doctor right away if you or a child in your care has symptoms of hepatitis C.
You May Like: Hepatitis B Foundation Drug Watch
Questions /false Answers At End Of References
Hepatitis C recurrence in liver grafts is rare
Fibrosis in hepatitis C infected liver grafts is accelerated when compared with native liver
Standard treatment for hepatitis C is effective after liver transplantation
Patients with hepatitis C infected liver grafts should be treated with large doses of corticosteroids after transplantation
Transplantation for hepatitis C related cirrhosis is becoming increasingly common worldwide
Obesity And Fatty Liver Disease
Obesity, and all of its related complications, is more serious than most adults in America believe. More than one-third of U.S. adults are obese. Obesity-related conditions include heart disease, stroke, type 2 diabetes, fatty liver disease, and certain types of cancer, are some of the leading causes of preventable death. We are seeing an increase in the number of young children and adolescents developing obesity, and all of the related complications.
The cost of obesity is staggering, with annual medical cost of obesity exceeding $147 billion in 2008 U.S. dollars. The medical costs for people who are obese were $1,429 higher than those of normal weight.
Dr. Galati and the Liver Specialists of Texas team are dedicated to evaluate, treat, and manage all aspects of obesity and non-alcoholic fatty liver disease , including the complication of cirrhosis and liver failure. Developing a customized plan of care for each patient they see is their objective.
Also Check: Is Hepatitis C Serious Disease
Future Directions And Needs
Despite the difficulties that the physician faces in the treatment of HCV infection, it cannot be ignored because of the vast number of patients it affects worldwide. Indeed, all efforts need to focus on better designed multicenter trials, instead of small, sporadic studies that leave conflicting trails and better diagnostic accuracy in distinguishing between recurrent HCV infection and acute cellular rejection. Some encouraging news may arise from the direction of new medications, such as new HCV protease inhibitors or long acting types of interferon, which may be combined in order to improve the results and, possibly, decrease the side effects45. These are being evaluated in ongoing human trials, initially in the pretransplant chronic HCV population, with the transplant data yet to come.
Posttransplant Followup And Monitoring Of Hcv Hepatitis Disease Progression
The risk of progression to cirrhosis can be predicted by the biochemical and histologic recurrence pattern. Aminotransferase peak, bilirubin level, and the presence of biochemical cholestasis are associated with a higher rate of progression to graft cirrhosis . Histologic findings from liver biopsies performed in the first 12 months after transplantation are useful for predicting the risk of developing cirrhosis, severity of fibrosis, and graft loss . The presence of histologic recurrence, including cholestasis and hepatocellular ballooning, at an early stage is associated with higher rates of progression to cirrhosis . Moderate-to-severe inflammation in liver biopsies performed within the first 12 months is also predictive of progression to cirrhosis and graft loss .
In this background, posttransplant monitoring with reliable methods is crucial for predicting patient/graft outcome, to make an early diagnosis of disease progression, and to start antiviral treatment at the appropriate time. There are two types of prevalent diagnostic methods for monitoring recurrent hepatitis C after liver transplantation invasive and noninvasive .
Don’t Miss: What Is Hepatitis B And What Causes It