Prophylactic Strategies Against Recurrent Hbv Infection After Olt
HBIG monotherapy. The efficacy of HBIG in prevention of recurrent HBV infection after OLT was first demonstrated in a large, retrospective, European multicenter trial . Among 359 patients who underwent liver transplantation for HBV infection, the risk of recurrent HBV infection 5 years after OLT was 75% among patients who received no or short-term HBIG therapy, compared with 33% among those who received HBIG for 6 months after transplantation .
Incidence of recurrent hepatitis B virus infection after orthotopic liver transplantation , by prophylactic regimen. Data adapted from . HBIG, hepatitis B immune globulin.
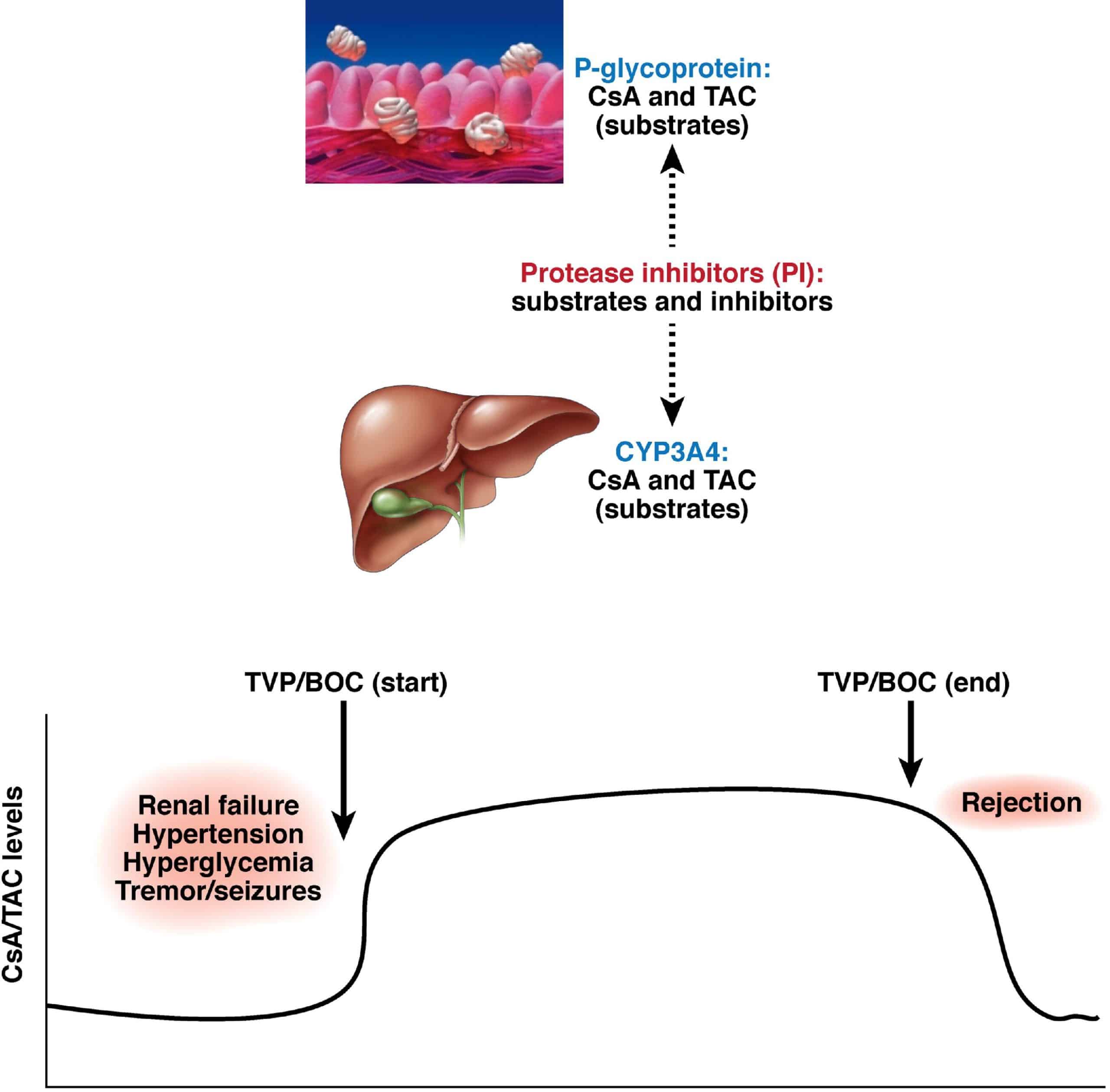
Overall, the results for lamivudine monotherapy are similar tobut no better thanthose for HBIG monotherapy for prophylaxis against recurrent HBV infection . As in the pre-OLT period, it is clear that the major limitation of lamivudine monotherapy is the development of resistant YMDD mutants. The rate at which these mutations emerge is higher after OLT than it is among patients who have not undergone transplantation. For this reason, the efficacy of lamivudine monotherapy in long-term prophylaxis after OLT is limited, and most transplantation centers currently advocate a combination of lamivudine with HBIG.
Treatment Of Chb After Lt
In CHB infection, complete eradication of HBV from the host is exceedingly rare. Even after hepatitis B surface antigen seroclearance, it is likely that HBV still persists within the host. This is the reason why lifelong antiviral therapy is required. Despite the removal of the liver, HBV may still persist in extrahepatic sites such as the lymph nodes, spleen, peripheral blood mononuclear cells, and other organs. HBV may also persist in the circulation at the time of transplantation. These sites serve as reservoirs for re-infection of the new graft. Furthermore, reactivation of latent HBV occurs with the use of immunosuppressive therapy after transplantation. Therefore, in the absence of effective antiviral therapy, severe hepatitis leading to graft failure from recurrent HBV infection is almost universal. In fact, prior to the advent of effective HBV therapy, liver transplantation was considered a contraindication because of untreatable HBV recurrence.
What Happens After Transplant Surgery
After the transplant surgery, you may need to stay in the hospital for several weeks while your health care team monitors how well your body is accepting the new liver. You’ll take medicines to control any pain. You will start taking immunosuppressive drugs to prevent your body’s immune system from rejecting the new liver.
If you have chronic hepatitis B infection, you will continue the antiviral drug therapy you had started before the transplant surgery to stop the virus from becoming active. Hepatitis B reactivation can be a very serious, sometimes even deadly, complication.
You will need the most medicines during the first 3 months after transplantation. It is important for you to be familiar with the medicines and to report any side effects. Not every patient having a liver transplant takes the same medicines or has the same side effects.
After a liver transplant, you will undergo regular blood tests and occasional liver biopsies to make sure your body is not rejecting the new liver. In addition, these tests will show whether the liver cancer is in remission or returning. It is very important that you closely follow the instructions from your transplant team.
Also Check: How Do People Get Hepatitis C
Prophylaxis With Alternative Dosing Schedules Of Hbig
The high economic cost of prophylaxis schedules combining HBIG plus oral antivirals, together with the high efficacy and safety of the more recent oral antivirals , have led to the study of different prophylactic strategies aimed at lowering or eliminating HBIG in order to reduce costs and the inconveniences associated with its administration.
Additionally, other possible routes of administration of HBIG have been assessed. Several studies have shown that low-dose intra-muscular administration of HBIG when combined with NAs is a cost-effective alternative to its intravenous administration. Recently the subcutaneous administration of HBIG has been found equally effective, well-tolerated, and accepted by patients.
These studies, therefore, show that IV administration of high doses of HBIG is neither necessary nor cost-effective when given together with oral antivirals and also highlight the importance of pretransplant levels of HBV-DNA as a predictive factor for recurrence.
Withdrawal of HBIG after combined prophylaxis: Studies of this strategy vary greatly in design, type of antiviral agent used, and time from LT to HBIG withdrawal. In addition, most of the studies are observational and from a single center, with just three randomized studies. The overall rates of recurrence in these studies ranged from 0% to 17%.
No studies are yet available concerning the combined use of two ANs as prophylaxis without HBIG.
What Is A Liver Transplant
With a liver transplant, the surgeon removes the diseased liver and replaces it with a healthy liver. A liver transplant is used for tumors that cannot be completely removed, either because of the size or location of the tumors or because the liver is too diseased for regular surgery. A transplant is possible only if the tumors are small and have not invaded nearby blood vessels.
The 5-year survival rate for patients who have had a transplant is between 60% and 70%. Before any liver transplant, the doctor will first test for possible hepatitis B or C infections. If you are infected with either hepatitis B or hepatitis C, you will be treated with antiviral medicines before the transplant. The antiviral medications will be continued after surgery for a certain amount of time to prevent your healthy liver from becoming infected.
You May Like: Can Hepatitis Be Transmitted Sexually
What Are The Common Conditions That Cause Someone To Need A Liver Transplant
Among adults in the U.S., the most common reason for a liver transplant is cholangitis caused by chronic hepatitis C, followed by cholangitis caused by long-term alcohol abuse. Many other diseases cause cholangitis, including the following:
- Other forms of chronic hepatitis, including hepatitis B and autoimmune hepatitis.
- NASH, or nonalcoholic steatohepatitis, a disease caused by a buildup of fat in the liver resulting in inflammation and damage to liver cells.
- Some genetic conditions, including Wilson disease where dangerous levels of copper build up in the liver, and hemochromatosis where iron builds up in the liver.
- Diseases of the bile ducts. Bile ducts are tubes that transport bile, a digestive liquid made in the liver, to the small intestine. These diseases include primary biliary cholangitis, primary sclerosing cholangitis, and biliary atresia. Biliary atresia, a disease of absent or malformed bile ducts usually identified shortly after birth, is the most common cause of liver failure and transplant in children.
Other reasons for liver transplantation include primary liver cancer, meaning cancers that originate in the liver, such as hepatocellular carcinoma.
Treatment Of Hbv Infection Before Liver Transplantation
There are several goals of antiviral therapy in patients with cirrhosis secondary to chronic HBV infection. In patients with compensated cirrhosis, antiviral therapy may prevent progression to decompensated cirrhosis and potentially eliminate the need for OLT. Antiviral therapy could also potentially reduce the risk of progression to hepatocellular carcinoma. In patients with decompensated cirrhosis, antiviral therapy may stabilize or even improve liver function, potentially delaying the need for transplantation. In patients whose conditions progress to the point at which transplantation is required, the goal of antiviral therapy is to minimize the HBV titer at the time of transplantation, thereby reducing the risk of recurrent HBV infection after OLT.
Studies of patients coinfected with HIV and HBV have demonstrated that reverse-transcriptase inhibitors used for treatment of HIV infection may also be highly active against HBV. Both tenofovir disoproxil fumarate and emtricitabine are approved for use against HIV infection and have demonstrated excellent antiviral activity against HBV in preliminary studies. In addition, tenofovir has demonstrated efficacy against lamivudine-resistant strains of HBV, without significant renal toxicity . The precise role of these agents in the treatment of hepatitis B, and the potential efficacy of nucleoside/nucleotide combination therapy have yet to be fully elucidated.
Recommended Reading: What R The Symptoms Of Hepatitis A
Treatment In Decompensated Cirrhosis And On Transplant Wait List
In those patients for whom liver transplantation becomes necessary, viral suppression ideally to undetectable levels remains important in preventing HBV recurrence in the graft. Studies have shown a direct correlation between viral load at time of transplant and rate of recurrence.19 This, in conjunction with post-transplant prophylaxis, which will be discussed later in this review, has resulted in HBV recurrence rates falling from 70% to 100% to < 10%.20
Shortening Duration Of Hbig Treatment By Replacing Hbig With Second Na At Various Time Points Post Olt
Four case series reported the discontinuation of HBIG with the addition of a second NA at various time intervals post OLT . Post-OLT HBsAg recurrence rates ranged between 6% and 12% in patients treated with the combination of adefovir and lamivudine. Other NA combinations including tenofovir and emtricitabine have also been used with similar outcomes . In our institution we reported 26 patients that were followed for 31.9 months after being switched to combination TDF/ETV. All patients had undetectable HBV DNA, and 24 patients remained HBsAg negative . In order to avoid cross-resistance most studies used a combination of nucleoside and nucleotide as prophylaxis. In majority of these studies there was considerable variability in the duration of use of HBIG anywhere from 7 days to 26 months post OLT.
More recently Radhakrishnan et al. reported a retrospective study of 42 patients who received a very short course of HBIG while in the hospital after liver transplantation. NA monotherapy was initiated prior to transplant and maintained indefinitely with tenofovir, entecavir, or tenofovir/emtricitabine. Major inclusion criteria included HBV DNA viral load less than 100 IU/mL within 3 months before transplantation, absence of resistance, hepatitis D infection, or HIV infection. One and 3 years cumulative incidence of recurrence, based on reappearance of HBsAg, was only 2.9% .
Recommended Reading: Symptoms Of Hepatitis C In Females
What Is A Living Donor Liver Transplantation
During a living donor liver transplant, a portion of a healthy persons liver is removed and transplanted into another person to replace their unhealthy liver. Both the donors and recipients livers will regrow over the next few months. Receiving a living donor transplant reduces the amount of time a person needs to wait on the national transplant waiting list.
What Happens During Transplant Surgery
Liver transplant surgery is complex. During the operation, surgeons will remove the entire injured or diseased liver and replace it with the donor liver. Several tubes will be placed in your body to help it carry out certain functions during the operation and for a few days afterward. These include a breathing tube, intravenous lines to provide fluids and medications, a catheter to drain urine from your bladder, and other tubes to drain fluid and blood from your abdomen. Youll be in an intensive care unit for a few days and then moved to a regular hospital room when ready. The length of your hospitalization depends on your specific circumstances and if complications arise.
You May Like: Hepatitis C Can You Get Rid Of It
How Does The Transplant Waiting List Work
Someone who needs a liver transplant is referred to a transplant center to be evaluated by a team of specialists from a variety of fields. Once the person completes all required testing, the transplant committee reviews the information. If the committee determines the person is a suitable candidate to receive a transplant, his or her name is placed on the national transplant waiting list. This list is managed by the United Network for Organ Sharing , which administers the Organ Procurement and Transplantation Network , responsible for transplant organ distribution in the U.S. The organ allocation system ensures that organs from deceased donors go to the sickest people first.
When people are put on the waiting list theyre assigned a priority score indicating how urgently they need a transplant. The score is calculated by their healthcare provider based on a specific formula. The two scoring systems are the MELD used for adults, and the PELD , used for children less than 12 years of age.
MELD scores range from 6 to 40 and are based on whether the person is on dialysis or not and the results of the following four blood tests:
- INR , an indicator of the liver making the proteins necessary for a persons blood to clot
- Creatinine, an indicator of kidney function
- Bilirubin, an indicator of liver health
- Sodium, an indicator of the bodys ability to regulate fluid balance
PELD scores range from negative numbers to 99 and are based on the:
What Happens During Liver Transplant Surgery
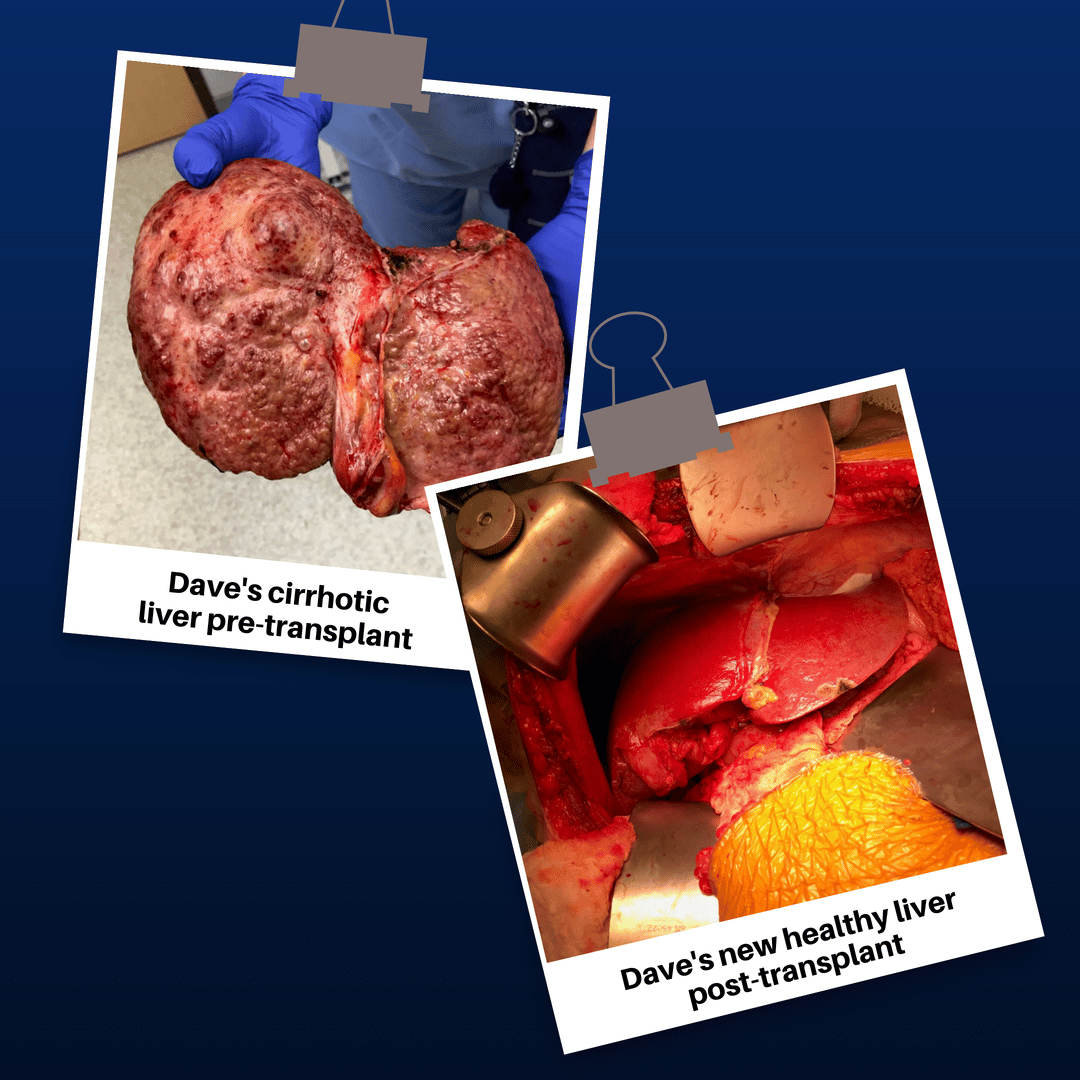
During transplant surgery, the transplant team replaces the diseased liver with a donated, healthy liver. The blood type and body size of the donor have to match the person receiving the transplant. Liver transplant surgery usually takes between 4 and 12 hours. Most patients stay in the hospital for up to 3 weeks after surgery.
You May Like: Hepatitis C Viral Rna Genotype Lipa
Injection Drug Use May Be Mostly To Blame Researcher Says
byZaina Hamza, Staff Writer, MedPage Today July 10, 2021
Hepatitis B virus was discovered in patients receiving liver transplants, despite donors testing negative for the virus, CDC researchers found.
From 2014 to 2019, the agency received reports of 20 patients who contracted HBV after liver transplants from donors who had no evidence of prior HBV infection, according to Danae Bixler, MD, and colleagues from the CDC.
History of injection drug use was the most common risk factor for HBV in 100% of participants from 2014 to 2018 and in 86% of those studied in 2019, the authors wrote in the Morbidity and Mortality Weekly Report.
“The increase in HBV donor-derived infections reported in 2019 among liver recipients might be related to increased numbers of donors with hepatitis C infection or recent injection drug use,” Bixler told MedPage Today.
She noted an increase in overdose deaths from opioids/stimulants during that time period, as well as an increase in liver transplants both from hepatitis C virus -seropositive donors and HCV RNA-positive donors currently infected with the virus.
For years, liver transplantation has been known as the most effective treatment option for chronic HBV-related liver failure, cirrhosis, and even hepatocellular carcinoma, but reactivation of HBV post-transplantation remains a clinical challenge affecting survival, the authors noted.
Disclosures
How Is Hepatitis B Diagnosed
A blood test will show if you have hepatitis B. Blood tests are done at a doctors office or outpatient facility. A blood sample is taken using a needle inserted into a vein in your arm or hand. The blood sample is sent to a lab to test for hepatitis B.
If you are at higher risk of getting hepatitis B, get tested. If you are pregnant, you should also get tested. Many people with hepatitis B do not know they are infected. Early diagnosis and treatment can help prevent liver damage.
A blood test will show if you have hepatitis B.
Your doctor may suggest getting a liver biopsy if chronic hepatitis B is suspected. A liver biopsy is a test to take a small piece of your liver to look for liver damage. The doctor may ask you to stop taking certain medicines before the test. You may be asked to fast for 8 hours before the test.
During the test, you lie on a table with your right hand resting above your head. Medicine is applied to numb the area where the biopsy needle will be inserted. If needed, sedatives and pain medicine are also given. The doctor uses a needle to take a small piece of liver tissue. After the test, you must lie on your right side for up to 2 hours. You will stay 2 to 4 hours after the test before being sent home.
A liver biopsy is performed at a hospital or outpatient center by a doctor. The liver tissue is sent to a special lab where a doctor looks at the tissue with a microscope and sends a report to your doctor.
Recommended Reading: How To Contract Hepatitis B And C
How Long Does It Take To Receive A Donor Organ
Its impossible to predict how long someone will have to wait for a new liver. Sometimes people wait only a few days or weeks before receiving a donor organ. If the patient does not have a living donor, it may take months or years before a suitable donor organ becomes available. Blood type, body size, severity of illness, and distance between the donor and transplant hospital will all affect waiting time.
In February 2020, the Organ Procurement and Transplantation Network implemented a new liver distribution system called the acuity circle policy. This policy emphasizes the medical urgency of liver transplant candidates and the distance between the donor and transplant hospitals. Livers from all deceased donors will first be offered to the most urgent liver transplant candidates listed at transplant hospitals within a radius of 500 nautical miles of the donor hospital. Following offers to the most urgent candidates, livers from adult donors will be offered to candidates at hospitals within distances of 150, 250 and 500 nautical miles of the donor hospital. These offers are grouped by medical urgency.
This new policy replaces the decades-old system of donation service areas and regional boundaries across the U.S. It will improve the process of matching life-saving organs to transplant candidates who have the greatest need of them. You can read more about the new national liver and intestinal organ transplant system by visiting the OPTN website here.
Liver Transplantation For Chronic Hepatitis B
Although LT is curative for decompensated cirrhosis, HCC, and liver failure, it does not eradicate HBV from a chronically infected host . It is well documented that HBV can reside in extra-hepatic sites and remain as a source of reactivation after LT. Even though the hepatocytes are the primary site of HBV DNA replication, viral replication outside has been demonstrated in pancreatic islet cells and renal proximal tubular epithelium. Furthermore, covalently closed circular DNA , the stable template for HBV replication, can be found in extra-hepatic tissues. Viral particles have also been demonstrated inside peripheral blood mononuclear cells, with the presence of cccDNA and active viral protein produced within lymphocytes. Therefore, strictly speaking, for a chronically infected patient after LT, the role of prophylaxis is to prevent reactivation, rather than re-infection or recurrence of HBV. The reason is because the recipient has never achieved complete or sterilizing cure with LT, and hence the need for life-long antiviral prophylaxis.
Don’t Miss: How Does One Catch Hepatitis B