What Is Hepatitis E
Hepatitis E, also called enteric hepatitis , is similar to hepatitis A, and more prevalent in Asia and Africa. It is also transmitted through the fecal-oral route. It is generally not fatal, though it is more serious in women during pregnancy and can cause fetal complications. Most patients with hepatitis E recover completely.
Treatments For Hepatitis C
Hepatitis C can be treated with medicines that stop the virus multiplying inside the body. These usually need to be taken for several weeks.
Until recently, most people would have taken 2 main medicines called pegylated interferon and ribavirin .
Tablet-only treatments are now available.
These new hepatitis C medicines have been found to make treatment more effective, are easier to tolerate, and have shorter treatment courses.
They include simeprevir, sofosbuvir and daclatasvir.
Using the latest medications, more than 90% of people with hepatitis C may be cured.
But it’s important to be aware that you will not be immune to the infection and should take steps to reduce your risk of becoming infected again.
Deterrence And Patient Education
Patient education is key to preventing and controlling hepatitis, especially viral and alcoholic hepatitis. Patients who have viral hepatitis must obtain education educated regarding the importance of routine follow-up and the importance of monitoring the disease progression and development of complications. They should learn about the importance of personal hygiene, including frequent handwashing. People who are traveling to endemic areas should be advised not to drink untreated water or ingest shellfish or raw seafood, and fruits and veritable should always be eaten after being cooked or after being peeled. Patients who have hepatitis A should not handle food for others until they stop shedding the virus. Patients should receive instruction about not sharing any articles, including toothbrushes, razors, or needles that have the potential for contamination with saliva, semen, or blood. All the patients should avoid using hepatotoxic agents, including alcohol and acetaminophen. Patients who are having a disease progression with liver disease should be referred to a gastroenterologist or hepatologist promptly. Patients with features of liver damage that includes liver fibrosis, cirrhosis, hepatocellular carcinoma, and features of portal hypertension should be monitored with routine labs.
Vaccination
Hepatitis A
Hepatitis B
Hepatitis C
Hepatitis D
Hepatitis E
Hepatitis G
Also Check: How Do You Get Hepatitis B And C
What Type Of Doctor Treats Hepatitis C
Hepatitis C is treated by either a gastroenterologist, a hepatologist , or an infectious disease specialist. The treatment team may include more than one specialist, depending on the extent of liver damage.Surgeons who specialize in surgery of the liver, including liver transplantation, are part of the medical team and should see patients with advanced disease early, before the patient needs a liver transplant. They may be able to identify issues that need to be addressed before surgery can be considered. Other persons who can be helpful in managing patients include dietitians to consult on nutritional issues and pharmacists to assist with management of drugs.
What Causes Hepatitis C
The hepatitis C virus causes hepatitis C. The hepatitis C virus spreads through contact with an infected persons blood. Contact can occur by
- sharing drug needles or other drug materials with an infected person
- getting an accidental stick with a needle that was used on an infected person
- being tattooed or pierced with tools or inks that were not kept sterilefree from all viruses and other microorganismsand were used on an infected person before they were used on you
- having contact with the blood or open sores of an infected person
- using an infected persons razor, toothbrush, or nail clippers
- being born to a mother with hepatitis C
- having unprotected sex with an infected person
You cant get hepatitis C from
- being coughed or sneezed on by an infected person
- drinking water or eating food
- hugging an infected person
- shaking hands or holding hands with an infected person
- sharing spoons, forks, and other eating utensils
- sitting next to an infected person
A baby cant get hepatitis C from breast milk.18
You May Like: How Do You Get Hepatitis A And B
Causes And Risk Factors
THe HCV virus causes hepatitis C.
People contract the virus through blood-to-blood contact with contaminated blood. For transmission to occur, blood containing HCV must enter the body of a person without HCV.
A speck of blood, invisible to the naked eye, can carry hundreds of hepatitis C virus particles. The virus is not easy to kill.
The CDC offers advice on cleaning syringes if it is not possible to use clean and sterile ones. Although bleach might kill the HCV in syringes, it may not have the same effect on other equipment. Boiling, burning, and using alcohol, peroxide, or other common cleaning fluids to wash equipment may reduce the amount of HCV, but it might not stop a person contracting the infection.
It is extremely dangerous to inject bleach, disinfectant, or other cleaning products, so be sure to rinse the syringe thoroughly. Only ever use bleach to clean equipment if new, sterile syringes and equipment are not available.
A person cannot contract the virus from casual contact, breathing, kissing, or sharing food. There is no evidence that mosquito bites can transfer the virus.
The report the following risk factors for developing hepatitis C:
- using or having used injectable drugs, which is currently the most common route in the U.S.
- receiving transfusions or organ transplants before 1992, which is before blood screening became available
- exposure to a needle stick, which is most common in people who work in healthcare
- being born to a mother who has hepatitis C
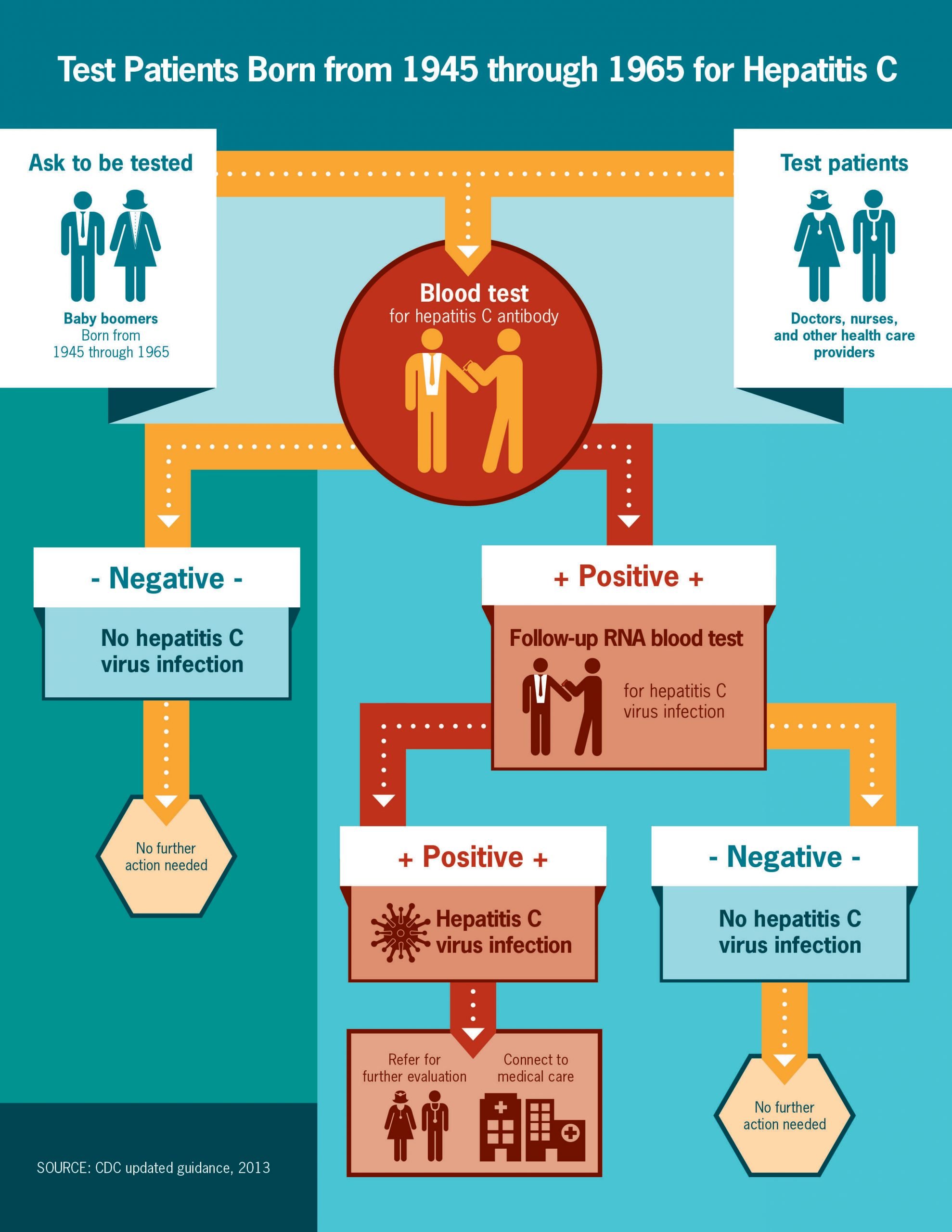
How Is Hepatitis C Diagnosed
Blood tests for hepatitis C
There are several blood tests for the diagnosis of hepatitis C infection. Blood can be tested for antibody to hepatitis C . It takes about 8-12 weeks on average, and up to 6 months, for antibodies to develop after the initial infection with hepatitis C, so screening for antibodies may miss a few newly infected individuals. Having antibodies is not an absolute indication of active, multiplying hepatitis C virus, but if the antibody test is positive , the statistical probability of active infection is greater than 99%.
Several tests are available to measure the amount of hepatitis C virus in a person’s blood . The hepatitis C virus’s RNA can be identified by a type of test called polymerase chain reaction that detects circulating virus in the blood as early as 2-3 weeks after infection, so it can be used to detect suspected acute infection with hepatitis C early infection. It also is used to determine whether active hepatitis is present in someone who has antibodies to hepatitis C, and to follow the viral load during treatment.
Blood tests are also performed to identify the genotypes of HCV. Genotypes respond differently to different treatment, so this information is important in selection of the most appropriate treatment regimen.
Estimation of liver fibrosis using blood tests also is quite reliable in diagnosing clinically significant scarring these include FIB-4, FibroSure, Fibrotest, and aspartate aminotransferase-to-platelet ratio index .
Don’t Miss: How Does Hepatitis C Affect The Liver
Complications Of Hepatitis C
If the infection is left untreated for many years, some people with hepatitis C will develop scarring of the liver .
Over time, this can cause the liver to stop working properly.
In severe cases, life-threatening problems, such as liver failure, where the liver loses most or all of its functions, or liver cancer, can eventually develop.
Treating hepatitis C as early as possible can help reduce the risk of these problems happening.
Viral Hepatitis Definition And Overview
Hepatitis means inflammation of the liver. Many illnesses and conditions can cause inflammation of the liver, for example, drugs, alcohol, chemicals, and autoimmune diseases. Many viruses, for example, the virus causing mononucleosis and the cytomegalovirus, can inflame the liver. Most viruses, however, do not attack primarily the liver the liver is just one of several organs that the viruses affect. When most doctors speak of viral hepatitis, they are using the definition that means hepatitis caused by a few specific viruses that primarily attack the liver and are responsible for about half of all human hepatitis. There are several hepatitis viruses they have been named types A, B, C, D, E, F , and G. As our knowledge of hepatitis viruses grows, it is likely that this alphabetical list will become longer. The most common hepatitis viruses are types A, B, and C. Reference to the hepatitis viruses often occurs in an abbreviated form The focus of this article is on these viruses that cause the majority of human viral hepatitis.
Hepatitis viruses replicate primarily in the liver cells. This can cause the liver to be unable to perform its functions. The following is a list of major functions of the liver:
Read Also: How Do You Contract Hepatitis A
What Is The Treatment For Viral Hepatitis
Treatment of acute viral hepatitis and chronic viral hepatitis are different. Treatment of acute viral hepatitis involves resting, relieving symptoms, and maintaining an adequate intake of fluids. Treatment of chronic viral hepatitis involves medications to eradicate the virus and taking measures to prevent further liver damage.
Acute hepatitis
In patients with acute viral hepatitis, the initial treatment consists of relieving the symptoms of nausea, vomiting, and abdominal pain . Careful attention should be given to medications or compounds, which can have adverse effects in patients with abnormal liver function . Only those medications that are considered necessary should be administered since the impaired liver is not able to eliminate drugs normally, and drugs may accumulate in the blood and reach toxic levels. Moreover, sedatives and “tranquilizers” are avoided because they may accentuate the effects of liver failure on the brain and cause lethargy and coma. The patient must abstain from drinking alcohol since alcohol is toxic to the liver. It occasionally is necessary to provide intravenous fluids to prevent dehydration caused by vomiting. Patients with severe nausea and/or vomiting may need to be hospitalized for treatment and intravenous fluids.
Chronic hepatitis
Medications for chronic hepatitis C infection include:
- oral daclatasvir
Medications for chronic hepatitis B infection include:
- oral entecavir
- oral tenofovir
Fulminant hepatitis
What Is Chronic Viral Hepatitis
Patients infected with HBV and HCV can develop chronic hepatitis. Doctors define chronic hepatitis as hepatitis that lasts longer than 6 months. In chronic hepatitis, the viruses live and multiply in the liver for years or decades. For unknown reasons, these patients’ immune systems are unable to eradicate the viruses, and the viruses cause chronic inflammation of the liver. Chronic hepatitis can lead to the development over time of extensive liver scarring , liver failure, and liver cancer. Liver failure from chronic hepatitis C infection is the most common reason for liver transplantation in the U.S. Patients with chronic viral hepatitis can transmit the infection to others with blood or body fluids as well as infrequently by transmission from mother to newborn.
You May Like: How Does A Person Contract Hepatitis
How Is Viral Hepatitis Prevented
Prevention of hepatitis involves measures to avoid exposure to the viruses, using immunoglobulin in the event of exposure, and vaccines. Administration of immunoglobulin is called passive protection because antibodies from patients who have had viral hepatitis are given to the patient. Vaccination is called active protection because killed viruses or non-infectious components of viruses are given to stimulate the body to produce its own antibodies.
Avoidance of exposure to viruses
Prevention of viral hepatitis, like any other illness, is preferable to reliance upon treatment. Taking precautions to prevent exposure to another individual’s blood , semen , and other bodily secretions and waste will help prevent the spread of all of these viruses.
Use of immunoglobulins
Immune serum globulin is human serum that contains antibodies to hepatitis A. ISG can be administered to prevent infection in individuals who have been exposed to hepatitis A. ISG works immediately upon administration, and the duration of protection is several months. ISG usually is given to travelers to regions of the world where there are high rates of hepatitis A infection and to close or household contacts of patients with hepatitis A infection. ISG is safe with few side effects.
Hepatitis A
Individuals at increased risk of acquiring hepatitis A are:
Some local health authorities or private companies may require hepatitis A vaccination for food handlers.
Hepatitis B
Hepatitis B vaccine is recommended for:
Who Is At High Risk And Should Be Tested For Hepatitis C Infection

The U.S. Preventive Health Services task force recommends that all adults born between 1945 and 1965 be tested once routinely for hepatitis C, regardless of whether risk factors for hepatitis C are present. One-time testing also is recommended for:
- People who currently inject drugs or snort drugs, or ever did so, even once many years previously
- People with persistently elevated alanine aminotransferase level, a liver enzyme found in blood
- People who have HIV infection
- Children born to HCV- or HIV-infected mothers
- People who were ever on long-term hemodialysis
- People who got a tattoo in an unregulated setting, such as prison or by an unlicensed person
- People who received clotting factor produced before 1987
- People who received transfusions or organ transplants before July 1992, or who were notified that they received blood from a donor who later tested positive for hepatitis C infection
- Health care, emergency medical, and public safety workers after a needlestick, eye or mouth exposure to hepatitis C-infected blood
People who may have been exposed to hepatitis C in the previous 6 months should be tested for viral RNA load rather than anti-HCV antibody, because antibody may not be present for up to 12 weeks or longer after infection, although HCV RNA may be detectable in blood as soon as 2-3 weeks after infection.
Also Check: Royal Canin Hepatic Wet Dog Food
Willowbrook State School Experiments
A New York University researcher named Saul Krugman continued this research into the 1950s and 1960s, most infamously with his experiments on mentally disabled children at the Willowbrook State School in New York, a crowded urban facility where hepatitis infections were highly endemic to the student body. Krugman injected students with gamma globulin, a type of antibody. After observing the temporary protection against infection this antibody provided, he then tried injected live hepatitis virus into students. Krugman also controversially took feces from infected students, blended it into milkshakes, and fed it to newly admitted children.
Alcohol And Other Toxins
Excessive alcohol consumption can cause liver damage and inflammation. This is sometimes referred to as alcoholic hepatitis. The alcohol directly injures the cells of your liver. Over time, it can cause permanent damage and lead to liver failure and cirrhosis, a thickening and scarring of the liver.
Other toxic causes of hepatitis include overuse or overdose of medications and exposure to poisons.
You May Like: What Happens To Your Body When You Have Hepatitis C
Hepatitis A B & C Disinfection Guidelines
Infection prevention is key in stopping the spread of Hepatitis A, B, and C, and other bloodborne pathogens. Cleaning and disinfecting items and surfaces that have been contaminated with blood or other bodily fluids can help lower the risk of being exposed to a bloodborne disease, including viral hepatitis, through cross-contamination.
Vital Oxide is an EPA-Registered Disinfectant that is tested and proven effective to kill several strains of viral hepatitis, including Hepatitis A, B, and C. Additionally, Vital Oxide meets surface disinfection recommendations from OSHAs Bloodborne Pathogen Standards for Hepatitis A, Hepatitis B, Hepatitis C, as well as HIV-1.
Here are some general disinfection steps to follow to reduce the spread of viral hepatitis.
What Is Hepatitis B
Hepatitis B is a more serious infection. It can lead to cirrhosis of the liver, liver failure, or liver cancer, causing severe illness and even death.
Hepatitis B virus spreads from person to person through blood or other body fluids. In the United States, this most commonly happens through unprotected sex with someone who has the disease or from injecting drugs with shared needles that aren’t sterilized. It also can be passed from an infected mother to her unborn baby.
The hepatitis B vaccine is approved for people of all ages to prevent HBV infection.
Read more about hepatitis B.
You May Like: Hepatitis B Surface Antibody Quantitative Titer
Explanation Of Test Results:
If this test result is positive, it means your body was exposed to the hepatitis C virus and made antibodies . However, it does not tell you whether you are still infected with hepatitis C. If the antibody test result is positive, you should be tested for hepatitis C RNA , which determines whether you are chronically infected. The lab will perform this RNA test automatically if your hepatitis C antibody test is positive.
If the antibody test result is negative, it means you have not been infected with the hepatitis C virus, and further testing for hepatitis C usually is not needed.
Acute Versus Chronic Viral Hepatitis
The term viral hepatitis can describe either a clinical illness or the histologic findings associated with the disease. Acute infection with a hepatitis virus may result in conditions ranging from subclinical disease to self-limited symptomatic disease to fulminant hepatic failure. Adults with acute hepatitis A or B are usually symptomatic. Persons with acute hepatitis C may be either symptomatic or asymptomatic .
Typical symptoms of acute hepatitis are fatigue, anorexia, nausea, and vomiting. Very high aminotransferase values and hyperbilirubinemia are often observed. Severe cases of acute hepatitis may progress rapidly to acute liver failure, marked by poor hepatic synthetic function. This is often defined as a prothrombin time of 16 seconds or an international normalized ratio of 1.5 in the absence of previous liver disease.
Fulminant hepatic failure is defined as acute liver failure that is complicated by hepatic encephalopathy. In contrast to the encephalopathy associated with cirrhosis, the encephalopathy of FHF is attributed to increased permeability of the blood-brain barrier and to impaired osmoregulation in the brain, which leads to brain-cell swelling. The resulting brain edema is a potentially fatal complication of fulminant hepatic failure.
Although some patients with cirrhosis are asymptomatic, others develop life-threatening complications. The clinical illnesses of chronic hepatitis and cirrhosis may take months, years, or decades to evolve.
Also Check: How Can You Contact Hepatitis C