Treatment Of Hepatitis C
Hepatitis C is treated with antiviral medications that aim to clear the virus from your body.
New all-tablet treatments have greatly improved the outcomes for people with hepatitis C. These treatments can cure more than 95% of individuals with chronic hepatitis C. There are several new tablets that are used in combination to treat all hepatitis C strains . They are effective for people with no liver damage and those who have more advanced liver damage or cirrhosis.
These new tablet medications are available and subsidised on the Pharmaceutical Benefits Scheme, and can be prescribed by specialists, general practitioners and specialised nurse practitioners.
There are no restrictions on accessing treatment it is available for all adults with a Medicare card. People under 18 are able to access treatment and it is recommended they are referred to a pediatrician experienced in the treatment of hepatitis C.
For more information on the new medications for the treatment of hepatitis C, see our video: Hepatitis C Cure what it means for Victorians.
If your doctor does not know about the new treatments, you can call the LiverLine on for information, and to find a GP who can help you.
Talk with your doctor about treatment options and the potential for interactions with other medications, herbal preparations and other drugs. If you take prescribed medication this will be managed so you can access treatment.
In general, if you have hepatitis C you will feel better if you:
What Other Tests Diagnose Hepatitis C
Once the diagnosis of hepatitis C is established, other tests may be done to determine whether the patient has developed liver fibrosis or scarring . This can be done with a needle biopsy of the liver, and examining the biopsied liver tissue under the microscope. Liver biopsy is less commonly done today because noninvasive tests are more readily available, more easily accomplished and less costly.
Liver imaging can evaluate fibrosis using ultrasound and MRI scans. Additionally, calculations using a variety of blood tests also can predict the degree of inflammation and fibrosis present. Genotype testing will typically be done to determine what subtype of hepatitis C the patient has, as this will impact what drugs are used for treatment.
Testing for other infections including HIV, hepatitis A, and hepatitis B is typically done to determine if the patient might have other conditions that could impact patient’s treatment and prognosis.
With the newest forms of antiviral treatment, the most common types of chronic hepatitis C can be cured in most individuals.
Diagnosis And Treatment Of Hcv Infection
Hepatitis C is rarely diagnosed at the time of infection, since few individuals are symptomatic. Asymptomatic cases may be detected, however, through recommended screening in high-risk populations, such as intravenous drug users and recipients of blood transfusions or organ transplants in which the tissues were not initially tested for HCV. Diagnostic testing and screening for hepatitis C centres on the detection of circulating antibodies and RNA specific to HCV. HCV RNA is detectable within 1 to 3 weeks of infection, and the antibodies are usually detectable within 8 to 12 weeks.
Treatment of hepatitis C is focused on the elimination of viral infection, improvement of liver function, and the prevention of cirrhosis and liver cancer. Liver function may be improved with the use of interferon, which reduces HCV replication and stimulates the immune system to fight HCV infection. Interferon is often given in combination with ribavirin, an antiviral drug that mimics nucleosides and thereby interferes with viral reproduction. Ribavirin may also be used in combination with agents known as sofosbuvir and velpatasvir, which inhibit key molecules involved in HCV RNA replication. Treatment of end-stage or advanced liver disease and cirrhosis caused by HCV infection is also possible with liver transplantation, though recurrence of detectable HCV infection is almost universal after transplantation.
You May Like: How Much Does A Hepatitis A Shot Cost
Hcv Genotypes/subtypes Dependent Transmission
The HCV genome demonstrated a prominent genetic diversity. Seven genotypes and 67 subtypes have been described. The genotypes are characterized by a distinct geographic distribution and clinical manifestations. For example, the genotype 1 is prevalent in Americas, Japan and Europe. Indeed, the HCV genotype prevalence also differs according to the transmission route and the age of infected individuals. For instance, the HCV gt 3a and 1a are highly represented among intravenous drug users and the HCV gt 1b is frequent among patients who received blood transfusions. In Japan, the HCV gt 1b is the most prevalent while, the infected population is generally older than in the United States, and an iatrogenic transmission is a predominant risk factor for the HCV acquisition.
Envelope Proteins E1 And E2
Glycoproteins E1 and E2 are type 1 transmembrane proteins that are forming the envelope of the virus particle .3B). E1 an E2 are cleaved from the precursor in ER by the cellular SP. The glycoproteins contained large hydrophilic ectodomains and 30 aa long transmembrane domains . The TMD is responsible for an anchoring of the envelope proteins in the membrane of the ER and their ER retention. The ectodomains of both glycoproteins are heavily glycosylated. The E1 has 4-5 and the E2 – 11 putative N-glycosylation sites, respectively. Interestingly, the glycosylation sites are rather conserved in each genotype, but the number of glycosylation sites varies between the genotypes. Its worth mentioning, that some of the glycans are engaged in folding and formation of the E1-E2 heterodimer complexes on the surface of the virion. These complexes are essential for the interaction with cellular receptors and helps to promote the virus-to-cell fusion.
Recommended Reading: How Long Does A Person Live With Hepatitis C
How Many People Have Hepatitis C
During 2013-2016 it was estimated that about two and half million people were chronically infected with HCV in the United States. The actual number may be as low as 2.0 million or as high as 2.8 million.Globally, hepatitis C is a common blood-borne infection with an estimated 71 million people chronically infected according to the World Health Organization .
How Can I Prevent Hepatitis C Infection
Although there is currently no vaccine to prevent hepatitis C, there are things you can do to avoid becoming infected or re-infected and prevent the spread of hepatitis C virus. Hepatitis C is not spread through food or close personal contact such as handshaking, hugging and kissing. Hepatitis C is spread when the blood from an infected person enters the bloodstream of an uninfected person. To avoid this happening:
- do not share needles or other equipment to inject drugs or any other substances
- do not use personal items that may have come in contact with an infected persons blood such as shavers or toothbrushes
- avoid touching blood or open wounds
- avoid sexual practices that might risk blood contact including trauma, during menstruation, or in presence of genital ulcers.
Recommended Reading: Can Alcohol Cause Hepatitis C
Extrahepatic Replication Of Hcv
The apparent presence of the HCV genomes in extrahepatic sites of patients infected with HCV has been shown. Using sensitive PCR assays, the HCV was revealed in leukocytes and there are evidences that these cells may represent a reservoir of the virus after treatment. Interestingly, the pool of the HCV quasi-species differs between the plasma and peripheral blood monocytes, suggesting an independent spread of HCV within different cell types. The infection of B-cells from non-Hodgkins lymphoma by HCV has also been demonstrated. A cell line established from transformed lymphocytes supported the HCV replication and also enable production of infectious viral particles capable to infect peripheral blood B cells. The significance of these extrahepatic HCV reservoirs is not well understood, although one could speculate that the leukocyte compartments might represent an additional route by which HCV can directly manipulate the immune system and also another means by which the virus avoids the eradication.
Hepatitis C Virus Strains
There are different strains of the hepatitis C virus. These are called genotypes. In New Zealand, it is estimated that of those infected with hepatitis C virus:
- 55% have genotype 1
- 35% have genotype 3
- 8% have genotype 2
- 1% have genotype 4 or 6.
It used to be important to know the genotype as it used to determine which treatment option was best. We now have a funded treatment called Maviret that treats all genotypes .
Also Check: How You Contract Hepatitis C
How Does The Hepatitis C Virus Spread
Hepatitis C is a blood-borne infection. It means that its risk increases when you get in contact with blood contaminated with the virus.
These are a few common ways of hepatitis C transmission:
- Sharing needles, syringes, or any equipment to inject drugs.
- An infected mother passing the virus to the child at the time of birth.
- Healthcare professionals not following proper hygiene practices.
- Getting tattoos or piercing in informal settings or with non-sterile instruments.
- Sharing personal items like razors, nail clippers, or toothbrushes.
- Through blood transfusion or organ transplants, especially which are before 1992.
- Having sex, especially if you have HIV.
Detection Of Viral Core Antigen
Compared to other diagnostic methods like EIA, the advantages of NATs are having higher specificity and sensitivity. However, the disadvantages of these assays are time-consuming and require sophisticated technical equipment, trained technicians, dedicated laboratory space and expensive reagents. In patients with HCV infection, it has been demonstrated that the HCV core antigen level strongly correlates with the HCV RNA level for various genotypes. Thus, due to cheap and easy-to-perform, the HCV core antigen quantification assay can be used as an alternative method to NATs to detect HCV RNA. Currently, core antigen detection by means of a chemiluminescent microparticle immunoassay can be fully automated in the Architect HCV Core antigen test . The Architect HCV Ag assay had a specificity of 100%, with a lower limit of detection of 3 fmol/L corresponds to approximately 1000 IU/mL of HCV RNA. Whereas,current HCV RNA assays have a lower level of detection between 5-15 IU/mL. In general, about 90% of HCV RNA positive samples are positive with a viral load above 10000 IU/mL, well in the sensitivity range of the HCV core antigen assay. Therefore, HCV antigen detection might be the next step following a positive antibody screening test. Several combination assays for detection of both anti-HCV antibodies and HCV core antigen have been developed.
Recommended Reading: Is There A Cure For Hepatitis C
Hepatitis C Antibody Test
Certain foreign substances that enter your body trigger your immune system to make antibodies. Antibodies are specifically programmed to only target the foreign substance they were made to fight.
If youve ever had a hepatitis C infection, your body will make hepatitis C antibodies as part of its immune response.
Your body only makes these antibodies if you have hepatitis C or had it in the past. So the hepatitis C antibody test can confirm whether you have the virus by testing for these specific antibodies.
It may take 2 to 3 months after exposure for the test to detect antibodies. If needed, your healthcare professional may order an HCV RNA test, which can detect the virus after just 1 or 2 weeks.
If the antibody test is positive, an HCV RNA test can show whether the infection is current.
While people of any gender experience the same hepatitis C symptoms, 2014 research suggested some effects of the virus may differ, depending on the sex you were assigned at birth.
Researchers noted that:
- women have a higher chance of clearing the virus without treatment
- liver disease may progress more rapidly in men
- men have a higher chance of developing cirrhosis
How Is Monitoring Done After Treatment For Hepatitis C
Once patients successfully complete treatment, the viral load after treatment determines if there is an SVR or cure. If cure is achieved , no further additional testing is recommended unless the patient has cirrhosis. Those who are not cured will need continued monitoring for progression of liver disease and its complications.
While cure eliminates worsening of fibrosis by hepatitis C, complications may still affect those with cirrhosis. These individuals still need regular screening for liver cancer as well as monitoring for esophageal varices that may bleed.
Because hepatitis B co-infection may reactivate or worsen even after treatment for HCV, monitoring for hepatitis symptoms may be needed after the end of therapy.
Also Check: Does The Hpv Vaccine Protect Against Hepatitis B
How Is Hepatitis C Treated
There are some very effective options for the treatment of hepatitis C infection. They are listed on the Medicare PBS , which makes them available at a much lower cost.
Newer treatments differ from those available previously:
- they cure more than 95% of people
- their side effects are minimal
- treatments last just 8 to 12 weeks
- they involve just a few pills each day, with no injections required
Curing hepatitis C means clearing the virus from the body. It helps reduce liver inflammation and can also help reverse scarring and cirrhosis. You can be re-treated if your treatment doesnt work the first time.
You should check with your doctor before taking any other medication or supplements, and whether you need vaccinations against hepatitis A and hepatitis B. You should also avoid alcohol if you have hepatitis. If you have liver damage, you may also need to see a liver specialist
For more information on how to get treatment, contact the National Hepatitis Info Line on 1800 437 222.
Who Should Be Screened For Hepatitis C
The United States Preventive Screening Task Force recommends screening for HCV infection in persons at high risk for infection due to life style factors or exposures. The USPSTF also recommends offering 1-time screening for HCV infection to adults born between 1945 and 1965.
A simple blood test is all that is required to find out if you have the virus. If you do have it, your doctor will order more tests to determine the âviral loadâ your blood contains and the extent to which your liver may be damaged.
You May Like: How Is Hepatitis C Transferred From Person To Person
What Is Autoimmune Hepatitis
Autoimmune Hepatitis is caused by a disorder of the bodys immune system. AIH occurs when the bodys immune system fights or attacks the liver cells. As a result of this attack, inflammation in the liver is caused. Medical research is still in the process of bringing out the clear cause of Autoimmune Hepatitis. It is believed that genetic and environmental factors can trigger inflammatory diseases.
There is no cure for this disease. Autoimmune Hepatitis is considered to be a deadly disease. If untreated, AIH may lead to serious liver problems, eventually leading to liver failure. However, if treated in the early stages, the symptoms can be put under control through medications and treatments. Liver transplantation surgery will be an option when AIH is not working for medications and treatments.
Alterations Of Lipid Metabolism
Lipids are required for the HCV replication and particles assembly. As mentioned above, HCV can modify the host serum lipid profile and this modification can provoke the steatosis. The steatosis is more frequent and more severe in patients with HCV gt 3 and it is correlated with a high HCV RNA levels. On one hand, in HCV-infected patients, the steatosis can be considered as a marker of the liver disease progression and, on the other hand, as an indication of the reduced response to therapy. However, if it is not metabolic or alcoholic steatosis, an efficient antiviral therapy is capable to reduce it.
Recommended Reading: Is Hepatitis C Sexually Transmitted Disease
What Are The Treatment Guidelines For Hepatitis C
Hepatitis C treatment is best discussed with a doctor or specialist familiar with current and developing options as this field is changing, and even major guidelines may become outdated quickly.
The latest treatment guidelines by the American Association for the Study of Liver Disease and Infectious Disease Society of America recommends use of DAAs as first-line treatment for hepatitis C infection. The choice of DAA varies by specific virus genotype, and the presence or absence of cirrhosis. In the U.S., specific insurance providers also might influence the choice due to the high cost of DAAs. Although the individual, public health, and cost benefits of treating all patients with hepatitis C is clear, the most difficult barrier to treating all people with HCV is the very high cost of the drug regimens. Patients are encouraged to discuss options with their health care professional.
Treatment is recommended in all patients with chronic hepatitis C unless they have a short life expectancy that is not related to liver disease. Severe life-threatening liver disease may require liver transplantation. Newer therapies with DAAs have allowed more and more patients to be treated.
What are the goals of therapy for hepatitis C infection?
The ultimate goals of antiviral therapy are to
- prevent transmission of hepatitis C,
- prevent progression to cirrhosis and liver cancer, and
- improve survival and quality of life.
What Type Of Doctor Treats Hepatitis C
Hepatitis C is treated by either a gastroenterologist, a hepatologist , or an infectious disease specialist. The treatment team may include more than one specialist, depending on the extent of liver damage.Surgeons who specialize in surgery of the liver, including liver transplantation, are part of the medical team and should see patients with advanced disease early, before the patient needs a liver transplant. They may be able to identify issues that need to be addressed before surgery can be considered. Other persons who can be helpful in managing patients include dietitians to consult on nutritional issues and pharmacists to assist with management of drugs.
Recommended Reading: How Can Hepatitis C Be Transmitted
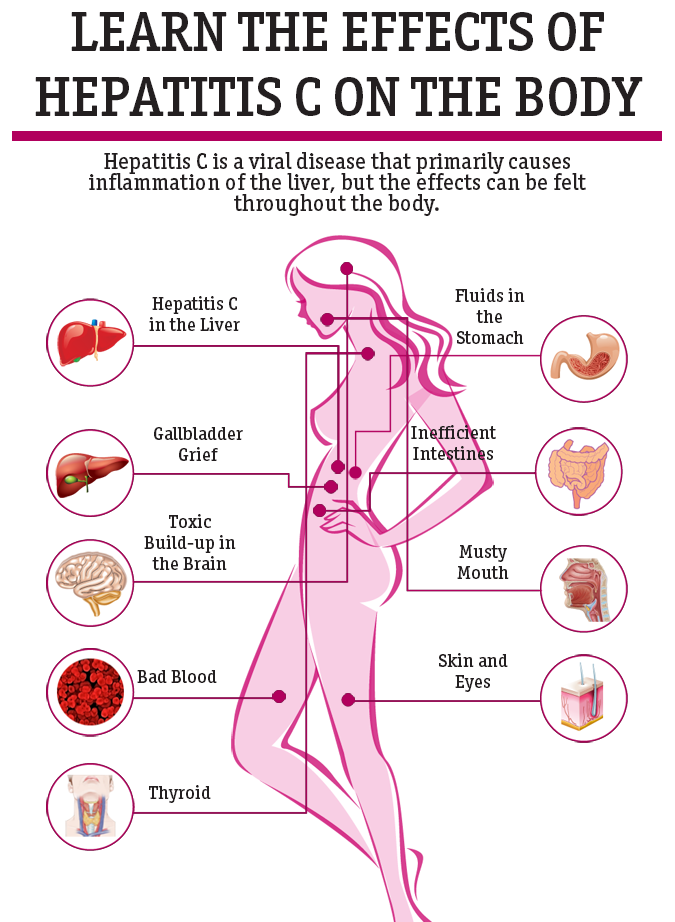
Causes Of Noninfectious Hepatitis
Although hepatitis is most commonly the result of an infection, other factors can cause the condition.
Alcohol and other toxins
Excess alcohol consumption can cause liver damage and inflammation. This may also be referred to as alcoholic hepatitis.
The alcohol directly injures the cells of your liver. Over time, it can cause permanent damage and lead to thickening or scarring of liver tissue and liver failure.
Other toxic causes of hepatitis include misuse of medications and exposure to toxins.
Autoimmune system response
In some cases, the immune system mistakes the liver as harmful and attacks it. This causes ongoing inflammation that can range from mild to severe, often hindering liver function. Itâs three times more common in women than in men.