What Are The Chances Of Persons With Hcv Infection Developing Long Term Infection Chronic Liver Disease Cirrhosis Liver Cancer Or Dying As A Result Of Hepatitis C
Of every 100 persons infected with HCV about:
-
75 to 85 persons may develop long-term infection
-
70 persons may develop chronic liver disease
-
15 persons may develop cirrhosis over a period of 20 to 30 years
-
Less than 3% of persons may die from the consequences of long term infection
-
Hepatitis C is a leading indication for liver transplants.
What Does It Mean To Get A False Positive For Hepatitis C
Hepatitis C Virus is one of the most common viruses in the world. HCV causes liver disease and cirrhosis. HCV infection may cause cirrhosis or liver cancer. Most cases are caused by sharing needles with someone who has hepatitis C. There are two types of HCV: 1) Hepatitis C virus type 1 , which is the main cause of chronic hepatitis 2) Hepatitis C virus type 2 .
A person infected with either type of HCV will have symptoms similar to those caused by other viruses such as flu, colds, chicken pox, etc. However, these infections do not usually lead to death due to antiviral treatment.
The most common symptom of HCV infection is jaundice, which occurs when the bodys white blood cells become overactive and produce too much bilirubin. Bilirubin builds up in the liver and causes yellowing of skin and eyes.
Other symptoms include fatigue, nausea, vomiting, abdominal pain, diarrhea and weight loss. These symptoms are often mistaken for some other condition such as viral hepatitis or bacterial endocarditis .
Once infected with type 1 or type 2 HCV, a person is likely to develop long-term infection. The rate of acute infection with either type of HCV does not differ much.
It is important to remember that not everyone infected with HCV develops a chronic infection. In fact, most people fight off the virus and develop antibodies against it.
These people are called acute HCV infection. Some people have a relatively mild infection that also leads to a quick recovery from the disease.
Why Take The Hepatitis C Virus Infection Test
The hepatitis C test is an essential tool for screening and diagnosing a hepatitis C infection. It can also help assess and monitor the treatment. The only way to detect if a person has a chronic hepatitis C infection is though a blood test: the HCV antibody test. This test can expose a past exposure and an active one but it cannot pinpoint whether the infection is current or past.
People who are at high risk of being infected with hepatitis C need to be tested for the hepatitis c antibodies. These include people who inject illegal drugs, those who have been on long term dialysis, kids who are born to HCV positive women, anyone who has been exposed to the blood of somebody who is infected with hepatitis C, anyone who has chronic liver disease, people who are HIV-positive, and health care workers who come in close contact with hepatitis C positive blood. This test is also recommended for anyone who has abnormal results on a liver panel.
Recommended Reading: How Can You Get Infected With Hepatitis B
Enzyme Immunoassays For Detection Of Hepatitis C Antibody
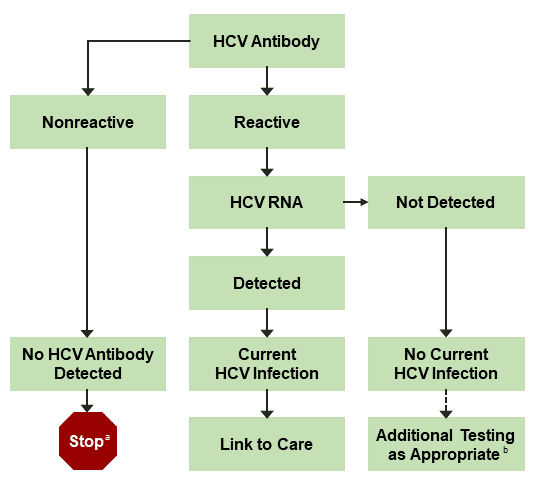
The HCV Ab test is used for initial screening for hepatitis C. The test is performed by enzyme immunoassays , which detect the presence of hepatitis C antibodies in serum. The result of the test is reported as positive or negative. Third-generation EIAs have a sensitivity/specificity of approximately 99%. However, the presence of HCV Ab does not indicate whether the infection is acute, chronic, or resolved. A positive antibody test result should be followed up with an HCV RNA test to confirm that viremia is present.
How To Get Tested
Hepatitis B testing is typically prescribed by a doctor and performed in a hospital, lab, or other medical setting. Taking a hepatitis B test requires a blood sample, which can be collected by a health care professional.
For laboratory-based testing, blood is drawn from a patientâs vein. After blood is collected, the sample is sent to a laboratory for analysis.
Also Check: How Can Hepatitis C Be Transmitted
Understanding Changes In Biomarkers During Disease Progression
Understanding the changes in HBV biomarkers over the course of a persons infection and recovery is key to interpreting the test results. Figure 3-1 and Figure 3-2 depict the typical biomarker changes over the course of hepatitis B disease.
Figure 3-1. Typical serologic course of acute hepatitis B to recovery
Figure 3-2. Typical serologic course of the progression to chronic hepatitis B
Acute, resolved, and chronic hepatitis BApproximately 90% of people > 5 years of age with acute hepatitis B will spontaneously clear their infection . People with resolved hepatitis B will remain positive for total anti-HBc and develop anti-HBs that protect against future HBV infection . Chronic hepatitis B is defined as an HBV infection lasting > 6 months. During the typical course of chronic infection, the total anti-HBc and HBsAg markers will always be present, whereas anti-HBc IgM will disappear . Hepatitis B envelope antigen and hepatitis B envelope antibody are variably present. HBV DNA levels vary during the course of chronic infection. Any detectable HBV DNA level is considered positive for surveillance purposes.
Among people with previously inactive hepatitis B , laboratory evidence of reactivation includes meeting any one of the following criteria:
- HBV DNA is now detectable or
- HBsAg test conversion occurs .
Who Should Get Tested For Hepatitis C
The CDC recommends that you get tested at least once no matter what. Definitely get screened if any of these things apply to you:
- You were born between 1945 and 1965.
- You use or inject drugs.
- You have ever injected drugs — even if it was just once or a long time ago.
- Youâre on kidney dialysis.
- You have abnormal alanine aminotransferase levels .
- You had a blood transfusion, blood components, or an organ transplant before July 1992.
- Youâve ever gotten clotting factor concentrates made before 1987.
- You received blood from a donor who later tested positive for hepatitis C virus.
- Youâre a health care worker, first responder, or have another job that exposes you to HCV-infected needles.
- You were born to a mother with HCV.
Read Also: What Does Hepatitis C Ab Non Reactive Mean
Hiv And Hbv Coinfection
About 2% of people with HIV in the United States are coinfected with HBV both infections have similar routes of transmission. People with HIV are at greater risk for complications and death from HBV infection. All people with HIV are recommended to be tested for HBV, and if susceptible, are further recommended to receive the hepatitis B vaccination or, if chronically infected, evaluated for treatment to prevent liver disease and liver cancer. For more information about HIV and HBV coinfection, visit HIV.govâs pages about hepatitis B and HIV coinfection.
Hepatitis C And Health
How can health-care personnel avoid exposure to HCV?
Avoiding occupational exposure to blood is the primary way to prevent transmission of bloodborne illnesses among health-care personnel. To promote blood safety in the workplace, health-care personnel should consult infectious-disease control guidance from the National Institute for Occupational Safety and Health and from CDC. Depending on the medical procedure involved, Standard Precautions may include the appropriate use of personal protective equipment .
What is the risk of acquiring hepatitis C after being accidentally exposed to HCV-contaminated blood or body fluids in the workplace?
Although sharps injuries have decreased in recent decades due to improved prevention measures, they continue to occur, placing health-care personnel at risk for several bloodborne pathogens like hepatitis C. A recent analysis of several studies revealed an overall 0.2% risk for infection among those exposed to HCV-antibody-positive blood through needlestick or sharps injuries . Updated guidelines for management and treatment of hepatitis Cexternal icon are available to provide guidance for health-care personnel who become infected via exposure to contaminated blood at the workplace.
Other than needlesticks, do other exposures place health-care personnel at risk for hepatitis C?
Should HCV-infected health-care personnel be restricted in their work?
Don’t Miss: How Do You Test For Hepatitis C
What Is Hepatitis B
Hepatitis B is a liver infection caused by the hepatitis B virus . HBV infection causes inflammation of the liver. When the liver is inflamed or damaged, its function can be affected.
- The best way to prevent HBV infection is by getting vaccinated. Safe and effective vaccines are available and covered as a preventive service by most health plans.
- For some people, HBV infection is an acute, or short-term, illness for others, it can become a long-term, chronic infection. Risk for chronic infection is related to age at infection: approximately 90% of infected infants become chronically infected, compared with 2-6% of adults.
- Chronic hepatitis B can lead to cirrhosis, liver cancer, liver failure, and premature death.
- Hepatitis B is diagnosed with a simple blood test that can detect HBV infection years before symptoms develop and the virus has caused liver damage.
- There is no cure for hepatitis B, but there are several FDA-approved medications that treat HBV infection. People with chronic hepatitis B should be monitored regularly for signs of liver disease and evaluated for possible treatment.
You May Like: Cure For Hepatitis A And B
Hepatitis B Blood Tests
The Hepatitis B Panel of Blood Tests
Only one sample of blood is needed for a hepatitis B blood test, but the Hepatitis B Panel includes three parts. All three test results are needed to fully understand whether a person is infected or not. Below is an explanation of the 3-part Hepatitis B Panel of blood test results.
Read Also: What Do You Do If You Have Hepatitis C
False Positive Hepatitis C Antibody Test Results In Left Ventricular Assist Device Recipients: Increased Risk With Age And Transfusions
Grace Y. Minamoto1, Doreen Lee1, Adriana Colovai2, Dana Levy1, Ljiljana Vasovic3, Keith W. Roach4, Jonathan Shuter1, Daniel Goldstein5, David DAlessandro5, Ulrich P. Jorde6, Victoria A. Muggia1
1 Division of Infectious Diseases, Department of Medicine, 2 Department of Pathology, Montefiore Medical Center and the Albert Einstein College of Medicine, Bronx, NY, USA 4Department of Medicine, Weill Medical College of Cornell University, New York, NY, USA Department of Cardiovascular and Thoracic Surgery, 6 Division of Cardiology, Department of Medicine, Montefiore Medical Center and the Albert Einstein College of Medicine, Bronx, NY, USA
Correspondence to
Keywords: Hepatitis C left ventricular assist device allosensitization
Submitted Sep 30, 2016. Accepted for publication Dec 28, 2016.
doi: 10.21037/jtd.2017.01.10
Hepatitis C Testing And Diagnosis
Doctors will start by checking your blood for:
Anti-HCV antibodies: This blood test is the first and sometimes only one you may get. Also called the ELISA screen, it checks for antibodies that your body releases to fight the virus. These are proteins your body makes when it finds the hep C virus in your blood. They usually show up about 12 weeks after infection. Your test will be either negative or positive for antibodies. It usually takes a few days to a week to get results, though a rapid test is available in some places.
What the results mean
Negative . This is when your blood shows no signs of HCV antibodies. Most of the time, thatâs because you never came in contact with the virus and you do not have hep C.
Sometimes, your negative result can be false, meaning you have HCV. That may happen if you:
- Took the test too soon after your exposure. This test checks for only HCV antibodies, which can take several months to appear.
- Have HIV, a donated organ, or other conditions that weaken your immune system, which can suppress your antibodies
- Get hemodialysis for kidney problems
If youâve been exposed in the last 6 months, youâll need to be retested.
Positive . This means youâve been infected with HCV. But false positives are surprisingly common. More than 1 in 5 people who test positive donât actually have hepatitis C. Possible reasons include:
What the results mean
Recommended Reading: Hepatitis C Antibody 0.1 Meaning
Don’t Miss: Is There A Cure For Hepatitis B
Discusses Physiology Pathophysiology And General Clinical Aspects As They Relate To A Laboratory Test
AIDS is caused by 2 known types of HIV. HIV type 1 is found in patients with AIDS or AIDS-related complex and in asymptomatic infected individuals at high risk for AIDS. The virus is transmitted by sexual contact, by exposure to infected blood or blood products, or from an infected mother to her fetus or infant. HIV type 2 infection is endemic only in West Africa, and it has been identified in individuals who had sexual relations with individuals from that geographic region. HIV-2 is similar to HIV-1 in viral morphology, overall genomic structure, and its ability to cause AIDS.
Antibodies against HIV-1 and HIV-2 are usually not detectable until 6 to 12 weeks following exposure and are almost always detectable by 12 months. They may fall to undetectable levels in the terminal stage of AIDS when the patients immune system is severely depressed.
Routine serologic screening of patients at risk for HIV-1 or HIV-2 infection usually begins with a HIV-1/-2 antigen and/or antibody screening test, which may be performed by various FDA-approved assay methods, including rapid HIV antibody tests, enzyme immunoassays, and chemiluminescent immunoassays. In testing algorithms that begin with these methods, supplemental or confirmatory testing should be requested only for specimens that are repeatedly reactive by these methods according to assay manufacturers instructions for use.
Finding The Cause Of A False
Since there are various reasons for false-positive results, individuals should speak with a doctor about the probable cause. Some may be due to human error, such as a technical or clerical oversight.
However, a false-positive result can also result from another condition, such as an STI or an autoimmune disorder. Autoimmune disorders that may cause false-positive results include lupus and rheumatoid arthritis.
Donât Miss: What Are The Side Effects Of Hepatitis
Don’t Miss: Can You Catch Hepatitis C From Sex
Cases And Clusters Of Potential Public Health Importance
Jurisdictions should review and analyze hepatitis B data regularly to identify cases and clusters of hepatitis B that merit further investigation. When resources are limited, these should be prioritized for investigation based on the degree of public health importance. The following are examples of high priority cases and clusters:
- People of childbearing age who are or have the potential to become pregnant, indicating the potential for perinatal transmission
- Children 24 months of age to detect perinatal transmission
- People in age and demographic groups for whom infection may be acute due to recent transmission, including those
- 70 years of age
Read Also: How Can I Tell If I Have Hepatitis C
How Could A Person Have Been Exposed To Hepatitis C
HCV is spread primarily by direct contact with human blood. For example, you may have gotten infected with HCV if:
-
You ever injected street drugs, that may have had someone else’s blood that contained HCV on them. With the opioid crisis we are facing, we are now seeing increased rates of new hepatitis C infection.
-
You received blood, blood products, or solid organs from a donor whose blood contained HCV.
-
You were ever on long-term kidney dialysis as you may have unknowingly shared supplies/equipment that had someone else’s blood on them.
-
You were ever a healthcare worker and had frequent contact with blood on the job, especially accidental needlesticks.
-
Your mother had hepatitis C at the time she gave birth to you. During the birth her blood may have gotten into your body.
-
You ever had sex with a person infected with HCV.
-
You lived with someone who was infected with HCV and shared items such as razors or toothbrushes that might have had his/her blood on them.
Also Check: Is Hepatitis C And Hiv The Same
Why A False Positive Happens
A doctor will consider two factors when reviewing the accuracy of a test result. These two factors are the tests specificity and sensitivity.
Specificity refers to the ability of a test to correctly identify those who do not have a disease. This is called the true negative rate.
Sensitivity reflects the ability of a test to correctly identify those who do have a disease. This is called the true positive rate.
According to a , third-generation anti-HCV tests have an average specificity of 97.5% to 99.7%. The sensitivity of these tests varies from 61.0% to 81.8%.
These findings indicate that anti-HCV tests detect true negatives more accurately than true positives .
A person may receive a false-positive test result if they have HCV antibodies from a previous active infection. They may have received successful treatment for this infection, or their body may have cleared it without treatment.
In either case, the antibodies from the previous infection can remain in the body and lead to positive results on anti-HCV tests.
False-positive results can also occur in children who had HCV transmitted to them during birth from a mother with hepatitis C virus infection.
Ultimately, a person who receives a positive result from an anti-HCV test may not have an active hepatitis C infection. This is why a doctor then typically performs another test the HCV RNA RT-PCR test before making a definitive diagnosis.
People who do not have hepatitis C can often prevent exposure to it by: